Sleep Apnea and Cardiovascular Disease
advertisement
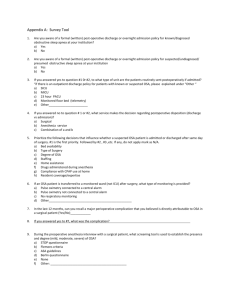
Obstructive Sleep Apnea and Cardiovascular Disease: A Tale of Two Unhappy Bedfellows Najib Ayas MD MPH Associate Professor of Medicine Sleep Disorders Program Critical Care and Respiratory Divisions University of British Columbia Multiple Lines of Evidence Suggest that OSA causes Cardio Vascular Disease (CVD) 1. Biologic Plausibility: Basic science/animal studies demonstrating a potential pathophysiologic link between OSA and CVD. 2. Associations: OSA is strongly and independently associated with CV Risk Factors and CVD in epidemiologic studies across many populations. 3. Experimental: Treatment of OSA leading to improved outcomes. Pathophysiology of Cardiovascular Disease Caused by OSA Recurrent upper airway obstruction Arousal From Sleep/Sleep Fragmentation Changes in Pleural Pressure/ Hemodynamic stress Activation of the Sympathetic Nervous System Oxidative Stress Activation of Systematic Inflammation Hypercoagulability Platelet Activation Hormonal changes Endothelial dysfunction Hypertension Acute strokes Heart failure Aortic Dissection Coronary events Glucose intolerance Obesity Hypoxemia/ Reoxygenation Animal studies Some have focused on simulating upper airway closure – Dogs with tracheostomies – English bulldog – Recent cat model different head positions Most are focused on the effect of intermittent hypoxia (IH) in rats/mice – Easier to do – Don’t reproduce all the aspects of human OSA – Degree of hypoxia greater than that commonly seen in patients with OSA – IH associated with oxidative stress, hypertension Intermittent Hypoxia and Atherosclerosis 40 mice exposed to 12 weeks of: CIH (12 hrs/day, 5% FiO2) plus high cholesterol diet CIH plus normal diet IA plus high cholesterol diet IA plus normal diet Savransy et al. AJRCCM 2007. Aortic plaques found 9/10 mice in CIH plus high cholesterol group Associated with increased lipids, increased markers of inflammation in the liver No plaques in other groups Human Studies: Presence of OSA Associated with a Variety of CV Risk Markers: Catecholamine levels CRP Endothelial dysfunction Leptin, adhesion Molecules (serum ICAM-1, sVCAM-1), Carotid intima media thickening Markers of oxidative stress 2. Association studies: Spanish study: 264 healthy men 377 snorers without sleep apnea 403 untreated mild/moderate disease 235 untreated severe disease 372 treated patients patients followed for 10 years for incident CVD (stroke,MI, PTCA, CABG) Marin et al, Lancet 2005 Fatal Cardiovascular Events Non-Fatal Cardiovascular Events Untreated severe OSA compared to healthy subjects: – increased odds ratio of fatal CVD by 2.87 (1.17-7.51) – nonfatal CVD by 3.17 (1.12-7.51) Odds ratios were not increased in treated patients Similar findings in older patients and women (unpublished) Epidemiologic Studies Linking OSA to Vascular Outcomes Aortic Dissection/Dilation: Kohler, Thorax 2009; Sampol AJRCCM 2003 Stroke : Arzt, AJRCCM, 2005; Yaggi, NEJM 2005 Myocardial Infarction: Peker, Eur Respir J, 2006 Sudden Cardiac Death: Gami, NEJM 2005 Atrial Fibrillation: Gami, Circulation 2004 Hypertension: Peppard, NEJM 2000 Major problem with non-randomized observational studies: Confounding – Confounding by indication/compliance – Other factors associated with sleep apnea and CVD Confounding? Cardiovascular Outcomes Central Obesity -Hypertension -Diabetes -Lipids Confounding by Indication/Compliance Sleep Heart Health Study Between 1995-1998, 6000 subjects enrolled in a variety of epidemiologic cardiovascular cohorts had PSG Followed for 9 years for incident CH disease (MI, revascularization, death from CHD) – Signal only in men <70 years (HR=1.10 for every 10 increase in AHI; for AHI>30, 68% increased risk) – Not in women, age>70 – Gottlieb et al. Circulation 2010 For stroke, – AHI>19 (4th quartile) had a HR of 2.86 for stroke in men – In women, association not as robust – Redline et al. AJRCCM 2010. ?Difference in community (survival) based vs. clinic cohort 3. Experimental Studies (RCT) in OSA: 1. short-term studies of surrogate endpoints 2. Measurements of atherosclerosis in carotid 3. long-term studies with clinically relevant endpoints • Stroke, heart attacks Surrogate Endpoints: BP Blood Pressure: Reasonable surrogate as it is highly correlated with future CV risks Effect consistent across most (but not all) drug classes CPAP (compared to the control group) reduces BP but effect is overall effect fairly modest (2 mm Hg) though effect greater in patients with more severe disease Majority of studies were less than one month AlAjmi et al, Lung 2007.; Haentjens, Arch Int Med, 2007 Two Recent Spanish RCT are consistent with these results Non-sleepy patients (ESS<11) with AHI>19/hr – 359 hypertensive patients randomized to CPAP vs. control for 12 months – Decreased systolic BP by 1.89 mm Hg, diastolic by 2.19 mm Hg (signal greatest if used CPAP>5.6 hrs/night) – Barbe et al. AJRCCM 2010. Patients with systemic hypertension and AHI>15/hr – Randomized 340 patients to CPAP vs. sham CPAP for 3 months – 24 hr systolic BP decreased by 2.1 mm Hg, diastolic by 1.3 mm Hg – Mean nocturnal BP decreased by 2.1 mm Hg – Duran –Cantolla et al. BMJ 2010. Other Surrogate Endpoints Positively Impacted by CPAP: Markers of inflammation (CRP), Metabolic derangements (glucose/insulin, lipids), oxidative stress markers, endothelial dysfunction Most of these outcomes have less robust independent associations with target outcomes than BP Most of these studied small numbers of subjects, were one month or less Many were non-randomized studies (before and after) Effects are inconsistent Direct Measurements of Atherosclerosis 24 patients with severe OSA Randomized to 4 months of CPAP vs. no CPAP After 4 months of CPAP: – Improved CRP, catecholamines – Reduction of CIMT with CPAP Drager et al. AJRCCM 2007. Long-term studies with clinically relevant outcomes: Many are ongoing: SAVE – 5000 person RCT (McEvoy, Australia) MOSAIC – Cardiac risk factors in non-sleepy patients with OSA (Stradling, UK) ADVENT – Sleep disordered breathing in patients with CHF (Bradley, Toronto) Other Unanswered Questions: Impact of Non-CPAP treatments for OSA in preventing CVD: – Dental appliances – Anti-oxidants – Statins – Weight loss Take-Home Message Accumulating data implicate OSA as a cause of CVD Larger RCT needed and in progress Consider treatment in: – Sleepy patients regardless of disease severity – In non-sleepy patients, consider treatment if: Moderate to severe sleep apnea (especially in the setting of hypoxemia) Underlying CVD/risk factors Treat underlying risk factors