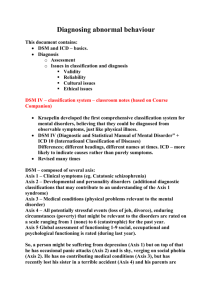
A2 unit 4 Clinical Psychology
advertisement
The DSM – how valid and reliable is it as a tool for diagnosis? A2 unit 4 Clinical Psychology Reliability of the diagnosis of schizophrenia Validity of the diagnosis of schizophrenia Pre-reading check • By now you should have an understanding of what the DSM is. • We now need to consider how reliable and valid it is. Learning outcomes: a) To be able to describe and evaluate the reliability of the diagnosis of Sz b) To be able to describe and evaluate the validity of the diagnosis of Sz c) To be able to describe and evaluate cultural issues in the diagnosis of Sz . (in all three cases using the findings of studies). • The Diagnostic and DSMStatistical Manual of Mental Disorder (Edition 5), was last published in 2013. • The DSM is produced by the American Psychiatric Association. • It is the most widely used diagnostic tool in psychiatric institutions around the world IV ICD - 10 • There is also the International Statistical Classification of Diseases (known as ICD). • It is produced by the World Health Organisation (WHO) and is currently in it’s 10th edition. DSM – a multi-axial system • Axis I • Axis II • Axis III • Axis IV • Axis V Disorders, clinical and mental eg schizophrenia Personality (underlying) including mental retardation Medical and Physical conditions Environmental factors Global functioning • • • • • Dad Purchased Most Extraordinary Glasses • The upcoming fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) makes several key changes to the category of schizophrenia and highlights for future study an area that could be critical for early detection of this often debilitating condition. Changes to the Diagnosis • Schizophrenia is characterized by delusions, hallucinations, disorganized speech and behaviour, and other symptoms that cause social or occupational dysfunction. For a diagnosis, symptoms must have been present for six months and include at least one month of active symptoms. • DSM-5 raises the symptom threshold, requiring that an individual exhibit at least two of the specified symptoms. (In the manual’s previous editions, that threshold was one.) Additionally, the diagnostic criteria no longer identify subtypes. Subtypes had been defined by the predominant symptom at the time of evaluation. But these were not helpful to clinicians because patients’ symptoms often changed from one subtype to another and presented overlapping subtype symptoms, which blurred distinctions among the five subtypes and decreased their validity. Some of the subtypes are now specifiers to help provide further detail in diagnosis. For example, catatonia (marked by motor immobility and stupor) will be used as a specifier for schizophrenia Evaluation of the DSM Strengths 1. Allows for common diagnosis (although many revisions) because it has stood the test of time When 2 or more doctors use the DSM, they should come close to the same diagnosis. 2. Evidence suggests that it is reliable ~Goldstein looked at the reliability between DSM-II and DSM-III is (1988) She found there was evidence of reliability within the DSM-III (but less so between DSM-II and DSM-III) Evaluation of the DSM Weaknesses 1. The DSM is seen as a confirmation of the medical state of mental disorder, as suffers are ‘patients’ and ‘treatment’ is suggested. Mental health issues are ‘disorders’ and ‘illnesses’ so ‘cures’ are looked for. However, it might be said that some mental disorders are simply ways of living …. who is to say whether it is ‘illness’ or not. (e.g. schizophrenics may be trying to get back to their normal self) Evaluation of the DSM Strengths: • It’s the best attempt at diagnosis that there is and it allows a common diagnosis • There are studies which support its reliability and validity Weaknesses • It can be considered a way of labelling people whose behaviour we see as “different” • In the US some people argue by inventing mental illnesses psychiatrists can make more money Reliability and the diagnosis of mental disorders The DSM’s reliability rests on the question of whether one person’s set of symptoms would lead to a common diagnosis by different physicians If different doctors give different diagnosis for the same set of symptoms (e.g. for the same person), then the diagnosis are not reliable and the treatment may not work Studies looking at the reliability of the DSM Goldstein (1988) • tested DMS-III for reliability and found that there was reliability • She looked at the effect of gender on the experience of schizophrenia • she re-diagnosed 199 patients, originally diagnosed using DSM–II; some differences • she asked two other experts to re-diagnoses (single blind) a random sample of 8 of the patients using the case histories with all indication of previous diagnoses removed • high level of agreement/consistency of diagnosis Goldstein (1988) • Goldstein realised that she was biased as she knew her hypothesis so she asked two experts to re-diagnose a random sample of 8 patients. • The experts received the original case notes with the diagnosis removed • She found a high level of agreement and interrater reliability. • This suggests that DSM-III is a reliable tool. Other research exploring Reliability • Using text books, research other studies that have explored the reliability of the DSM • What have these studies shown? Rosenhan (1973) use for reliability and validity • Because the diagnosis was the same across all 12 of the hospitals presumably using the current DSM at the time, we could say this shows the DSM to be reliable • Because the diagnosis of healthy people was schizophrenia, if they were using the DSM this means it lacks any validity Evaluation of validity issues STRENGTHS • The DSM has been shown to be valid across a variety of studies covering a range of different conditions • Because it is reliable it is likely to be valid too • Much work has been done to increase its validity as it has been rewritten WEAKNESSES • It is hard to diagnose people who are suffering from more than one condition (comorbidity) when using the DSM • It can be considered to be reductionist to break down a condition into a series of symptoms, so we shouldn’t over concentrate on Axis 1 • Questionnaires and interviews such as in the Kim-Cohen study may find what they are looking for CULTURAL ISSUES and the DSM Culture does not affect diagnosis Culture does affect diagnosis • It’s scientific, and if we clearly define our symptoms then it can work all over the world eg Lee(2006) in Korea • Schizophrenia is more similar across cultures than different • Some times symptoms mean different things in different cultures eg hearing voices can make you “special” in a positive way (spiritual) • There are cultural differences in symptoms • Eg more auditory hallucinations in Mexico, more grandiosity in white Americans, What should we do about the cultural problems in using the DSM? •We should be aware of the cultural problems in diagnosis •Concentrate less on first rank (positive) symptoms which tend to be more cultural •Concentrate more on negative symptoms which are less culturebound and easier to measure objectively Kirk and Kutchins (K&K) (1992) • In their review paper Kirk and Kutchins argued that there are methodological problems with the studies used to test the reliability of the DSM up until 1992… these then limit the generalisability of the findings. • The studies outlined used interviews and questionnaires to gather data; K&K argued that training and supervision of interviews was insufficient and that they lacked the commitment and skills to be accurate. They also pointed out that the studies they looked at tended to take place in specialised research settings… meaning that their findings might not relate to clinicians in normal clinical settings. Generally speaking, an unreliable diagnostic tool would lack validity…. K&K suggested the DSM could also lack validity. Evaluation of K&K (1992) points Points about interviewing - such as that different interviewers may affect the situation and lead to different data – might be important when considering generalising findings from studies Goldstein (1988) did not, however, use interviewing to test reliability – she used re-diagnosis using secondary data, and also found reliability Evaluation of K&K (1992) points The patients in the studies looked at were not all from research settings The ‘gamblers’ in Stinchfield’s study were on a gambling treatment program, not in a research situation. The patients in Brown et al.’s study were out patients in a hospital = possible ecological validity? Evaluation of K&K (1992) points • K&K’s study took place before Brown et al. and Stinchfield’s studies which showed that DSM-IV-TR could be regarded as reliable. Possible to therefore conclud that further work has been done since DSM-II and reliability has improved. • Goldstein (1988), Brown et al. (2003) and Stinchfield (2003) all provide evidence that diagnosis is reliable. Questions: you also have questions in your pack ~ page 5 that need to be completed 1) What do these studies tell us about the reliability of the DSM in diagnosing mental disorders? 2) How are Kirk and Kutchin’s findings different from the majority of the other studies? What does this tell us about the reliability of the DSM? 3) How can the reliability of the DSM be improved? Validity and the diagnosis of mental disorders • If the DSM were not reliable it would not be valid either. • If a diagnosis was done again and the DSM provided a different one, then it would not be a valid diagnosis (it would not be measuring what it claimed to measure) so therefore reliability and validity go together Validity and the diagnosis of mental disorders Outline what is meant by each of the following terms: – Construct validity – Etiolical validity – Concurrent validity – Predictive validity – Convergent validity Construct validity • If the DSM is to define mental disorders, then mental disorders need to be operationalised. Lists of symptoms and behaviour are the result of making a mental disorder measurable. • It has been argued that in operationalising a concept such as depression, something is lost from the understanding of the nature of the whole experience of depression, which means that the DSM is not a valid tool. There is a lack of construct validity, in that the constructs drawn up, for example to represent depression, might not be representative enough. Etiological validity If it has etiological validity, a group of people who have been diagnosed with the same disorder will have the same symptoms or factors causing it. e.g. schizophrenia is sometimes caused by too much of the neurotransmitter dopamine…. …..so in order to have etiological validity, people diagnosed as schizophrenic should all have an excess of dopamine in their brain Concurrent validity • For a diagnosis to have concurrent validity, symptoms that form part of the disorder but are not part of the actual diagnosis, should be found in those diagnosed. e.g. schizophrenics often have problems with personal relationships, but this is not a characteristic that is looked at when diagnosing them according to the classification system. Predictive validity • Predictive validity is present if diagnosis can lead to a prediction of future behaviours caused by the disorder. • If a diagnosis has predictive validity we should be able to say whether the person is likely to recover or whether the symptoms will continue • It should also be possible to predict how someone with a specific disorder will respond to specific treatments. e.g. the drug lithium carbonate is effective for bipolar disorder, but not effective for other mental disorders. If a classification system has good predictive validity and diagnoses someone with bipolar disorder, they should respond to lithium carbonate. Convergent validity • Convergent validity is when a test results converges on (gets close to) another test result that measures the same thing. • A correlation test would be carried out ~ If two scales measure the same construct, for example, then a person’s score on one should converge with (correlate with) their score on the other. Difference between convergent, predictive and concurrent • Convergent validity ~ the 2 measures should be measuring exactly the same thing • Predictive and concurrent can have different ways of measuring each case Task • Complete the gap fill sheet regarding the many types of validities relevant to the DSM. • Check your answers with the person beside you or ask for the answer sheet. Studies looking at the validity of the DSM • Next, in pairs read one of - Studies looking at the validity of the DSM from Kim-Cohen (2005), Hoffmann (20020 or Lee (2006) • For the chosen study read it and then report back to the class on what they found. • Evaluate the strengths and weaknesses of the validity of the DSM. Strengths – validity of diagnosis • The studies show the DSM is valid in its diagnosis. Different mental health issues were cited in the different studies, which reinforces the conclusion. It is likely that symptoms for disorders are well established, given that the DSM has had many revisions. Different research methods have yielded data that also match the DSM criteria. Strengths – validity of diagnosis • The claim that the DSM is valid is supported by the claim that it is reliable, as reliability and validity go together. If the DSM is not reliable it will not be valid. • Great efforts have been made to make the DSM-IV-TR more valid, such as adding culture-bound syndromes. Weaknesses – validity of diagnosis • It has been said that co-morbidity – the state of having more than one mental disorder – is hard to diagnose using the DSM, a system which relies on the user choosing the one closest match from lists of symptoms and features. • It could be claimed that splitting a mental disorder into symptoms and features is reductionist and that a holistic approach might be more valid. Weaknesses – validity of diagnosis • It is possible that the questionnaires and interviews produce the findings they are searching for. For instance, if it is well known that ‘children with ADHA are impulsive and hyperactive’, and teachers know which children have that label, they will then say, ‘those children are impulsive and hyperactive’. The diagnosis is selffulfilling. Cultural issues • Culture does not affect diagnosis – mental disorders are ‘scientific’ • The DSM was developed in the USA and is used widely in many other cultures. It is valid if mental disorders are clearly defined with specific features and symptoms. • Mental disorders are scientifically defined illnesses that are explained in a scientific way. Cultural issues • Culture does affect diagnosis – a spiritual model • There are studies that have shown that culture can affect diagnosis. • e.g. symptoms that are seen in western countries as characterising schizophrenia (such as hearing voices) are interpreted in other countries as showing possession by spirits, which renders someone special in a positive way, not a negative ‘disorder’. • Depending on cultural interpretations of what is being measured, the DSM is not always valid. • A clinician from one culture must be aware that a patient from another culture is guided by their own frame of reference. Questions 1) What are the two main theories surrounding culture and diagnosis of mental disorders? Be able to outline each. 2) Using your Student book, outline what two studies regarding culture and diagnosis of mental disorders. Homework • Research schizophrenia – what are three symptoms of this mental disorder?