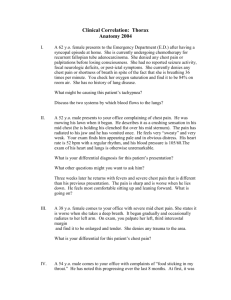
Thoracic Surgery Back to Basic
advertisement

Thoracic Surgery Back to Basic FM Shamji 2008 Esophagus Adult - hollow muscular tube 25 cm long 1 cm in neck, 19 - 22 cm in the mediastinum, 3 cm in the abdomen Specialized sphincters at each end LES – physiological sphincter, prevents gastroesophageal reflux UES – anatomical sphincter, prevents air entry during breathing and regurgitation from esophagus into pharynx Esophagus Three Heart burn Dysphagia Chest pain Three symptoms operations Antireflux repair Esophagectomy Esophageal myotomy Dysphagia Difficulty in swallowing is a WORRYING symptom; precise symptom that must never be ignored Clinical history is most important Progressive dysphagia with progressive weight loss are suggestive of malignancy Intermittent dysphagia implies motility disturbance Investigations must be thorough and quick First comes diagnosis, then comes treatment Investigations for Dysphagia Focused clinical history, present and past Physical examination is of secondary importance – begin with mouth, examine neck for supraclavicular lymph nodes, goitre, abdomen for hepatomegaly, ascites CXR Barium swallow and UGI study Upper GI endoscopy and mucosal biopsy Esophageal function assessment – manometry study if motility disorder is suspected CT scan chest and abdomen Implications of Delayed Diagnosis Failure to thrive and weight loss Recurrent aspiration pneumonia Bronchiectasis Lung abscess Lung fibrosis Empyema Retention esophagitis Local extension of cancer Aortic-esophageal fistula Tracheal-esophageal fistula Dysphagia – Case 1 1. 2. 3. A barium swallow was performed on this elderly 80-year-old man who had difficulty in swallowing. What is the diagnosis? What are the two important reasons for treatment? What treatments are possible? Zenker’s Diverticulum Pharyngoesophageal Diverticulum in the Neck Dysphagia and Recurrent Pulmonary Aspiration Treatment is always Surgical Cricopharyngeal Myotomy Myotomy alone (if small) Myotomy plus diverticulectomy (if large) Acquired condition – 80% of patients are >50 years age Pulsion diverticulum Dysfunction of the UES – cricopharyngeus muscle Other symptoms are: regurgitation of undigested food, choking and foul breath Dehiscence of Killian Dysphagia – Case 2 The barium study shown was obtained in a 55 year old man with a 10 year history of mild vague postprandial “indigestion” and heartburn. Within the past 6 weeks he has developed dysphagia for solid food and 10 lb weight loss. What is the next step in his management? Mid-Esophageal Stricture Cancer until proven otherwise Assessment of patient Complete history and physical examination Heart, Lung, Liver and kidney function Assessment of stricture Esophagoscopy and mucosal biopsy Rigid and flexible bronchoscopy CT scan chest and abdomen PET scan Esophageal U/S Causes of Esophageal Cancer Adenocarcinoma Barrett’s epithelium complicating chronic gastroesophageal reflux disorder Squamous cell carcinoma Excess alcohol and tobacco Nitrosamines in pickled vegetables and cured meats Silica in wheat Fungus Caustic ingestion Achalasia Chronic iron deficiency Tylosis palmaris et plantaris Remote radiation therapy to the mediastinum Gastro-Esophageal Reflux Disorder Backward flow of gastric juice into the esophagus Physiological and Pathological Lower esophageal sphincter is incompetent Causes Most common is idiopathic • Normal LES pressure 15 to 30 mmHg • <6 mmHg pathognomic reflux disorder • <10 mmHg reflux often present After treatment for Achalasia • Pneumatic dilatation or distal esophagomyotomy Scleroderma Esophagogastrectomy Truncal vagotomy and pyloroplasty Prolonged Naso-gastric tube insertion Symptoms of Gastroesophageal Reflux Disorder Typical symptoms Intermittent, substernal discomfort or burning sensation Within 1 hour of eating, with exercise or recumbent Postural regurgitation is most consistent symptom Water brash Atypical symptoms Cough, laryngitis, wheezing, pulmonary due to aspiration Dental caries due to loss of enamel Complications of Pathological GERD Esophagus Proximal airway Laryngitis Asthma Lung Reflux esophagitis Chronic blood loss – iron deficiency anemia Peptic stricture Epiphrenic diverticulum Barrett’s epithelium – risk for adenocarcinoma True Barrett’s ulcer – perforate into mediastinum, thoracic aorta, pericardium, and airway, penetrate, bleed massively Recurrent aspiration pneumonia – fibrosis, bronchiectasis, lung abscess, empyema Mouth – loss of tooth enamel Esophagus Which of the following tests is the most sensitive for the detection of pathologic gastroesophageal reflux? a. b. c. d. e. acid perfusion (Bernstein) test barium swallow 24 hr pH monitoring esophagoscopy manometric testing discussion 24 hour pH monitoring is now the gold standard and the most precise measurement of acid reflux. Normal pH range 4.1 and 7.0 Reflux episode is present when pH < 4.0 Endoscopic examination to assess acid-related esophageal mucosal damage – esophagitis, stricture, columnar metaplasia Barium swallow is for anatomical examination of esophagus, stomach and duodenum – demonstrate diverticula, hiatus hernia, esophageal stricture – a road map for safer endoscopic examination Manometric testing of esophagus is done for suspected motility disorder as a cause of dysphagia and chest pain Acid perfusion test will only confirm that esophagus is sensitive to acid – an attempt to reproduce symptoms Investigations for GERD CXR Barium study Hiatus hernia Stricture Zenker’s diverticulum Flexible esophagogastroscopy and mucosal biopsy Fixed hiatus hernia Pulmonary parenchymal changes from recurrent aspiration Hiatus hernia Esophagitis Columnar lined esophagus – look for Barrett’s epithelium from biopsy Esophageal function assessment Manometry Impedance-pH study 24 hr pH monitoring Complication of GERD A 45-year-old man presents with a history of recurrent heartburn with occasional central chest pain, and frequent episodes of postural regurgitation of gastric juice into his mouth. UGI endoscopy finding is shown. What is the diagnosis? Was it necessary to take mucosal biopsy? How will the diagnosis influence future treatment? Columnar Lined Esophagus Acquired condition due to chronic gastroesophageal reflux Barrett’s Epithelium – intestinal metaplasia recognized by presence of goblet cells Malignant transformation to adenocarcinoma Surveillance is important once dysplasia is present High grade dysplasia is serious; within 2 years adenocarcinoma develops Esophagus A 40-year-old man has progressive dysphagia and 20 lb weight loss for 6 months. He had taken antacids regularly for many years for heartburn and indigestion. Esophagoscopy performed for assessment is shown. Can you describe the findings? Are any other tests necessary for assessment of this lesion? What is the best treatment? Adenocarcinoma of Esophagus Columnar lined esophagus and distal malignant stricture Esophageal mucosal biopsy, CT scan chest and abdomen or PET scan, esophageal ultrasound, complete blood count and serum biochemistry Esophagectomy and reconstruction if patient is operable and cancer resectable Esophagectomy Esophageal Cancer Incidence of adenocarcinoma is rising – an explosion Gastroesophageal reflux related – not necessarily acid reflux Develops in metaplastic Barrett’s epithelium or heterotopic gastric mucosa in esophagus Always do mucosal biopsy of gastric cardia and distal esophagus – establish diagnosis of reflux and columnar transformation Esophagus A 50-year-old woman complains of nocturnal regurgitation and cough, a sour taste in her mouth, postural regurgitation, and heart burn for 5 years. She wants to consider an operation now. Which of the following is/are helpful in deciding whether to perform antireflux surgery? 1. 2. 3. 4. 5. failure of medical therapy to control symptoms incompetent lower esophageal sphincter presence of reflux related esophageal mucosal injury increased esophageal exposure to gastric juice. all of the above Emergency in Esophagus A 67-year-old man has had intermittent dysphagia, burning epigastric pain and retrosternal chest pain after meals for 2 years. For the past 24 hours, he has been unable to tolerate anything by mouth. CXR was done in the ER. What is the diagnosis? Does this condition constitute an emergency? Can you describe treatment that is most appropriate? Emergency in Esophagus 82-year-old woman Retrosternal chest pain, vomiting and retching for 48 hours Similar episodes in the past 4 years Emergency in Hiatus Hernia Risk of Volvulus and Strangulation in incarcerated Type III or IV hernia Early operation is mandatory to preserve stomach and prevent death from ischemic gastric necrosis and perforation Emergency Room Insert naso-gastric tube to decompress of stomach Intravenous fluid resuscitation with Ringer’s Lactate UGI Endoscopy to evaluate gastric mucosa • Stomach non-viable ---- urgent gastrectomy • Stomach viable ---- semi-urgent hiatus hernia repair and concomitant antireflux repair Type I Type II Type III Type IV Hernia Treatment for Hiatal Herniation Type I • Most common 85 to 90% • Operate for severe reflux disorder refractory to optimal medical therapy for minimum of 6 months Type II • Pure type II is rare < 1%. Operate to prevent mortality from strangulation and ischemic perforation Type III • Mixed Type I and II • More common than Type II 6% • Needs operation for symptoms of reflux and incarceration Type IV • Least common. Entire stomach in the chest with volvulus • Needs operation Management of GERD Medical Therapy is for life Diet must be modified eating small meals and avoid late night meals Antacids Combination of histamine receptor blocker PM dose and proton pump inhibitor AM dose Postural therapy by elevating head of bed 15 cm Surgical Therapy is for failure of medical therapy Anti reflux fundoplication Thoracic Surgical Emergency A 45 year old man, after a large meal and alcohol, arrives in the ER complaining of severe retrosternal and left pleuritic chest pain for 6 hours after a bout of vomiting and retching. Respiration 28, Pulse 130, BP 90/60, T 38.5 The most likely cause of his illness is 1. Aortic dissection 2. Acute pericarditis 3. Myocardial infarction 4. Pulmonary embolism 5. Esophageal perforation Barium Swallow Esophageal Perforation Very serious; high mortality is directly related to delay in treatment Acute septic mediastinitis and sepsis syndrome Iatrogenic is more common than post-emetic perforation Operation within 1 hour - resuscitation, drainage of sepsis in the mediastinum and pleural space, adequate repair of perforation, broad spectrum antibiotic for both aerobes and anaerobes, and nutritional support Dysphagia This barium swallow was performed on a 33-year-old woman complaining of difficulty in swallowing both solids and liquids for 4 years with gradual worsening over time and 10 lbs weight loss. Regurgitation of undigested food has occurred. What is demonstrated in this xray? How is this diagnosis confirmed? What is the treatment? Esophageal Motility Disorder Achalasia with Epiphrenic Diverticulum Esophagoscopy is necessary to assess gastroesophageal junction – rule out peptic stricture, leiomyoma, cancer Esophageal manometry confirms diagnosis Preferred treatment - Distal esophagomyotomy and partial fundoplication Pneumatic dilatation carries a risk of esophageal perforation of 4% Achalasia Achalasia is Greek for “without relaxation” in which the lower esophageal sphincter fails to relax before the oncoming bolus of food Failure of the sphincter to open is due to lack of the necessary stimulus of the peristaltic wave Motility disorder, neurogenic in origin, related to changes in the ganglion cells of the Auerbach’s plexus – degeneration, impaired function, query autoimmune in origin Chronic condition in which treatment is for palliation of obstruction to swallowing Manometric Features Achalasia: Manometric Features Definitive Diagnosis Achalasia LES Elevated baseline >45 mm Hg Incomplete Relaxation* RP>8 mm Hg Normal UES and Upper 1/3 striated segment of esophagus ESOPHAGEAL BODY Absent peristalsis* Elevated baseline Complications of Achalasia Esophageal Trachea Obstruction from compression due to mega-esophagus Pulmonary Progressive dilatation Retention esophagitis Perforation Epiphrenic diverticulum Malnutrition Squamous cell cancer pretreatment and adenocarcinoma posttreatment due to reflux Recurrent aspiration pneumonia, lung abscess, bronchiectasis, fibrosis Social Withdrawn, eats alone Pseudo-Achalasia due to Cancer in Gastric Cardia Mediastinum This specimen was removed from anterior-superior mediastinum in a 45-year-old woman complaining of fluctuating weakness in arms and legs, slurring of speech, chewing difficulty, drooping of eyelids. What is it? How could it have been predicted? Why was it removed? What condition does the patient have? Chest Radiograph Thymus Gland Thymus gland with a thymoma CT scan chest Presence of tumour and for treatment of muscle weakness Myasthenia Gravis Myasthenia Gravis Autoimmune disorder Auto-antibodies against acetylcholine receptors Reduced number of receptors destruction>synthesis Relationship to Thymus gland • Atrophic 10% • Thymoma 8% to 15% • Hyperplasia 70% to 80% Mediastinum The syndrome most commonly associated with a thymoma is a. b. c. d. e. Myasthenia gravis Red blood cell aplasia Aplastic anemia Hypogammaglobulinemia Cushing’s syndrome Parathymic Syndromes Myasthenia gravis Myositis dystrophica Myocarditis Dilated cardiomyopathy 12% Mucocutaneous candidiasis Non-thymic malignancies Red cell aplasia Hypogammaglobulinemia 30-45% Favourable prognostic factor 5% Autoimmune hemolytic anemia Hemoptysis Coughing up blood Differentiate between hemoptysis, hematemesis, epistaxis, bleeding from gums Clinical assessment CXR Bronchoscopy Chest CT scan Massive or Life-Threatening Hemoptysis The Ottawa Experience 90 Patients F. M. Shamji MBBS, FRCSC, FACS Division of Thoracic Surgery Ottawa Hospital University of Ottawa, Canada Airway Hemorrhage Definition MASSIVE HEMOPTYSIS Cause of Death Asphyxiation > 600 mL blood loss in 24 hours EXSANGUINATING HEMOPTYSIS > 1000 mL blood loss in 24 hours > 150 mL blood loss per hour Hypotension and Asphyxiation Asphyxiation It takes only 150 mL of blood in the bronchial tree to produce lifethreatening hypoxemia, if it is brisk DEAD SPACE VOLUME The Outcome of Significant Airway Hemorrhage Rate of Bleeding and Underlying Lung Function versus Timely Specific Treatment Airway Hemorrhage - Etiology I Cause of Bleeding Number of Cases (42) Lung Cancer 20 Lymphoma 2 Bronchiectasis 10 Retained aspirated foreign body 2 Acute pulmonary tuberculosis 1 Tracheo-innominate artery fistula 1 Lung abscess 3 Mycetoma 3 Airway Hemorrhage - Etiology II Cause of Bleeding Vascular Number of Cases (48) 22 Catheter related pulmonary artery rupture 10 Erosion of subclavian artery – mucormycosis 1 Aortobronchial fistula – thoracic aortic aneurysm 1 Erosion of prosthetic aortic graft 4 AV Malformation – bronchial, pulmonary 1,5 Post FNA – thrombocytopenia 1 Post bronchoscopic biopsy 1 Unknown 2 Airway Hemorrhage - Etiology Third World Population N=123 cases of Life-Threatening Hemoptysis Inflammatory Lung Disease N=101 Active pulmonary tuberculosis 47 Bronchiectasis 23 Chronic necrotizing pneumonia 11 Source of Bleeding in Significant Airway Hemorrhage Bronchial arterial circulation Non-bronchial arterial circulation Pulmonary arterial circulation Thoracic aorta Innominate artery Lung Cancer in USA - 2004 New Cases Rank Deaths Rank Male 93,110 2 91,930 1 Female 80,660 2 68,510 1 Total 173,770 3 160,440 1 Cell Types Small cell 25% Non-small cell 75% 50% adenocarcinoma 30% squamous cell 15% large cell undifferentiated 5% bronchiolaveolar, mixed adenosquamous Risk factors Tobacco smoking - greatest risk factor Prior surgery for lung cancer Occupational exposure to asbestos, uranium and nickel mining Prolonged exposure to high-level of radon – ubiquitous radioactive gas A history of other previous head and neck cancer High dose ionizing radiation Molecular Genetics Carcinogens in Tobacco Smoke Polycyclic aromatic hydrocarbons -benzopyrene Polonium 210 Phenol derivatives • 87% of lung cancers occur in active smokers • Amount of daily smoking • Tendency to inhale • Duration of smoking habit • 10-fold to 60-fold greater risk in smokers compared to non-smokers Diagnosis CT scan chest Bronchoscopy for central mass, atelectasis Fine needle aspiration biopsy for peripheral lung lesion Sputum cytology Cavitating lung mass A 55-year-old man is complaining of persistent cough and mild hemoptysis for 2 months. CXR is shown What is the differential diagnosis? What tests will be helpful in establishing diagnosis? Solitary Pulmonary Nodule A 39 year old man with recent onset of severe headaches and depression is found to have a 3 cm nodule in the RUL. He has been a 1 pack per day smoker for 24 years. What are the causes of SPN? How will you establish the diagnosis? CT scan Brain Lung FNA biopsy confirmed adenocarcinoma What additional tests are necessary? How much delay in management is acceptable? Which services need to be consulted? Right Arm Pain A 55-year-old man has pain in the right arm, anterior chest and axilla for 6 months. He has smoked for 25 years. Treated for shoulder bursitis, cervical spine disease, muscle strain What do you think he has? What tests will you order? Pancoast Tumour FNA biopsy lung lesion CT scan chest, abdomen, head MRI chest and head Nuclear bone scan PET scan Bronchoscopy and cervical mediastinoscopy to complete staging Pancoast Tumor Mass at the extreme apex of the lung within thoracic inlet area Pain Intercostal nerves Lower Brachial plexus C8 and T1 Bone invasion – ribs, vertebral body Horner’s syndrome Advanced local tumour-invasion through intervertebral foramen into spinal canal, higher brachial plexus, subclavian vessels Staging of Lung Cancer Why stage cancer? • Staging determines treatment • Staging determines prognosis • Staging allows assessment of efficacy of treatment for each stage of the disease • Staging allows comparison of treatment for different stages of disease between different centres Staging of Cancer Pre-operative • • • • • • Clinical assessment CXR CT scan chest, upper abdomen, and head Nuclear bone scan FNA – lung, neck lymph node if palpable, new skin nodule, soft tissue mass Mediastinal lymph node biopsy – cervical mediastinoscopy and left anterior mediastinotomy • Bronchoscopy – lobar obstruction, tracheal carina involvement Intra-operative • Lung mass – location, size, relationship to fissures and visceral pleura • Pleural space • Lymph nodes Post-operative • Surgical pathology – tumour cell type, differentiation and size, resection margins, visceral pleura invasion, lymph node status, local invasion parietal pleura and/or ribs • Follow-up for minimum 5 years Non-Small Cell Lung Cancer Staging Treatment for NSCLC Stage Localized IAB + IIAB Intention Treatment Cure Surgery + CT; add CT to increase by 10 – 15% for IB and II Loco-Regional IIIA + IIIB Depends Induction + Surgery Concurrent CT + RT CT alone Metastatic IIIB Pleural + IV Palliative BSC +/- CT Treatment for Non-small cell lung cancer Surgical and it must be Complete Resection Stage Ia and Ib –Surgery Stage IIa and IIb – Surgery Stage IIIa – potentially surgical, needs induction therapy Stage IIIb – potentially not surgical Stage IV – not surgical but one exception when it is stage IV only in the brain, the brain metastasis is solitary and resectable, and the primary tumour in the lung is localized and mediastinum is normal Small Cell Lung Cancer 20-25% of cell types <1% occur in non-smokers Most common cause of paraneoplastic syndromes – SIADH (water intoxication), ectopic ACTH (biochemical cushing’s syndrome), neuropathies, Eaton-Lambert syndrome Aggressive cancer, often advanced disease at presentation – stage IV Most chemo-sensitive and radio-sensitive Small Cell Lung Cancer Staging Very Limited Disease Confined only to one lung Mediastinum is normal Limited Disease Confined only to one lung and nearby lymph nodes, broncho-pulmonary and/or mediastinal Extensive Disease Intra-thoracic spread beyond one lung and lymph nodes or extra-thoracic spread Recurrent Disease Tumor has recurred in the same lung and/or another part of the body Small Cell Carcinoma Chemotherapy and/or radiotherapy Very limited disease • induction chemotherapy and then surgery Limited disease • confined to the ipsilateral chest – lung and mediastinum within field of radiotherapy • Without treatment fatal within 4 to 6 months • With treatment median survival 22 months and/or cured Extensive disease – systemic • Without treatment fatal within 12 to 14 weeks • With treatment median survival 10 to 12 months Para-neoplastic manifestations TRAUMA: A KILLER ON THE LOOSE “The public feels that if they go into any emergency room, they are in the hands of Jesus. They don’t realize how true that is.” Trauma takes its toll “ They often arrive in the middle of the night – when the streets are angry and the dark city terrors stalk innocent prey. Or mangled in highway accidents. Or badly injured in accidents at home or work. They are trauma victims. And most of them won’t live to see the coming of dawn. Thoracic Trauma Chest injuries account for 50% of civilian deaths due to trauma • 25% direct cause of fatality • 25% contributing factor <15% of patients with chest injury need urgent chest operation >85% are adequately treated by resuscitative measures, assisted ventilation, and inter-costal chest drainage Thoracic Trauma Loss of function is the abnormality Normal function of the Thorax Protection of internal viscera Preservation of vital function Lung ventilation, perfusion, and gas exchange, Cardiac pump, tissue perfusion, and oxygen transport Damaged organs loss of normal function Thorax is the vital pump Thorax the Vital Pump Requirements for Normal Respiration Normal respiratory centre and neuromuscular mechanism Chest wall that is both intact and mobile Intact ribs, sternum and diaphragm Pleural cavity that is not encroached upon Lungs that are both mobile and resilient Unobstructed air passages Normal alveolar-capillary membranes Thorax the Vital Pump Requirements for Normal Circulation Normal myocardium Intact cardiac valves and septa Normal intrinsic cardiac rhythm Normal pericardial space Adequate blood volume Normal sympathetic response Adequate oxygenation and normal acid-base and electrolyte balance Why is Thorax the Vital Pump? All life depends on oxygen-a constant supply that is needed at a rate of 250ml/min at rest and more in illness For every 1 ml of oxygen used up, 0.8ml of carbon dioxide is produced – a waste for the human body that must be regulated Constantly fighting acidosis –to maintain pH 7.4 requires integrated function: circulation, respiration, buffer system, and renal function Thoracic Trauma Pathophysiology – Disturbance of function Acute chest wall pain Changes in chest wall compliance and mechanics Unstable chest wall Chest wall defect Altered pleural pressures Increased work of breathing Lung parenchymal damage Retained bronchial secretions Acute cardiovascular alterations Airway injury Rib Fracture A single rib fracture in patient with pre-existing compromised lung function may precipitate respiratory failure Severe emphysema Paralyzed hemi diaphragm Previous extended pulmonary resection Acute chest wall pain Impaired cough Retention of secretions Atelectasis and V/Q mismatch Respiratory failure Consider Thoracic Trauma on Anatomical Basis Familiar with anatomy of the thorax Chest wall • • • • Soft tissues Ribs, single or multiple Pleura Sternum and Thoracic Spine Internal structures • • • • • Lungs Heart Major vessels Esophagus Diaphragm Consider Thoracic Trauma on Anatomical Basis Cannot dissociate a specific chest injury from one or more injuries of neighbouring structures Diaphragm rupture • Pelvic bone fracture • Lower rib fractures • Abdominal visceral injury: Liver on right, Spleen on left Fracture of sternum • Thoracic aortic rupture • Myocardial contusion • Thoracic spine fracture at T4 – T5 Flail chest injury • Multiple rib fractures • Hemothorax and/or pneumothorax • Lung contusion Thoracic Trauma Important Direct cause in 25% Contributing cause in 25% Early mortality is related to Hypoxia Hypotension Late cause of death mortality is related to Sepsis Multiple organ failure Priorities in Thoracic Trauma Establish patent airway Restore circulation and oxygen transport Occlude sucking chest wound Drain pleural space Re-expand lungs Stop bleeding Stabilize chest wall Evaluate ventilation – arterial blood gases Seven Immediately LifeThreatening Chest Injuries Proximal Airway Obstruction Open Pneumothorax Flail Chest Massive Hemothorax Tension Pneumothorax Cardiac Tamponade Air Embolism Six relatively Life-Threatening Chest Injuries Tracheal-Bronchial rupture Pulmonary Contusion Diaphragmatic rupture Major vascular injury Esophageal Perforation Myocardial Contusion Chest Trauma A 55 year old man involved in a car accident has been placed on assisted ventilation because of severe head injury. He was noted to have bruising and surgical emphysema on the right lateral chest wall but no pneumothorax. The ventilator setting is rate 16/min, tidal volume 500 mls, FIO2 of 40%, and PEEP of 10 cm of water pressure. He develops sudden tachycardia, hypotension, increase in airway pressure, and hypoxia. The most likely cause is a. b. c. d. e. open pneumothorax systemic air embolism cardiac tamponade tension pneumothorax myocardial contusion Chest Trauma The most common physiologically significant injury resulting from blunt chest trauma is a. b. c. d. e. flail chest pulmonary hematoma subcutaneous emphysema pulmonary contusion diaphragm rupture Chest Trauma A 24-year-old man is brought into the ER after a fall from a ladder. His breathing is laboured, and he is cyanotic. He is complaining of right chest pain. There is subcutaneous emphysema on the right side. No breath sounds can be heard in the right lung field, which is hyper-resonant to percussion. Among the following choices, the most appropriate next step in his management is: a. obtaining a stat chest X-ray b. insertion of an endotracheal tube c. cricothyroidotomy d. stat arterial blood gas analysis e. immediate needle decompression followed with chest tube insertion Indications of Severity in Chest Trauma Multiple rib fractures Sternal fracture 1st rib fracture Diaphragm rupture Flail chest injury Open pneumothorax Massive hemothorax Laryngeal fracture Open Pneumothorax Penetrating wound of the chest wall Ipsilateral lung collapse Inability to generate negative intra-thoracic pressure Often concomitant lung parenchymal injury Acute ventilatory failure Treatment: in the ER apply occlusive dressing over the chest wall wound or endotracheal intubation and assisted ventilation Penetrating Chest Wall Wound Open Pneumothorax Pathophysiology Open Pneumothorax Sucking chest wound Chest wall is breached and pleural space has become real. Open pneumothorax acute ventilatory failure Acute life-threatening state; act fast in the ER Cover defect with sterile occlusive dressing immediately followed by chest tube insertion Immediate endotracheal intubation and assisted ventilation Open Pneumothorax - Disturbance of Respiration Breach in Chest Wall If breach in chest wall is large these effects death occurs rapidly I f breach in chest wall is small, effects are less serious and outcome will depend on vital capacity Adhesions in pleural space will prevent lung collapse and so minimize these effects. Airway Obstruction A A AIRWAY A A Acute airway obstruction kills in 5 minutes Airway Obstruction Foreign body, vomitus or blood in the oropharynx Severe maxillofacial trauma Fracture of the larynx Treatment Remove foreign body from mouth Suction out blood or vomitus Establish airway by controlled intubation Cricothyroidotomy in selected cases Blunt Laryngeal Injury Chest Trauma: Emergency Airway Options Oro-tracheal or naso-tracheal intubation (stabilize C-spine) Fibre-optic Intubation Cricothyroidotomy Flail Chest Injury Damaged painful unstable chest wall Impaired cough Impaired breathing Retained secretions retention atelectasis V/Q mismatch hypoxia Inefficient ventilation Lung contusion Hemorrhagic, edematous, non compliant lung increased capillary permeability V/Q mismatch hypoxia Abnormal pleural space with pneumothorax and/or hemothorax compressive atelectasis V/Q mismatch Flail Chest Management of Flail Chest Injury Isolated injury or component of multiple injuries Severe chest injury Fractures of multiple ribs at two or more sites Recognized by paradoxical respiration Treatment: multiple injuries Control ventilation and correct hypoxia Pain control, relieve hemo-pneumothorax, restrict fluids Treatment: isolated injury Admit to a monitored location trauma unit or intensive care unit Optimum pain control, physiotherapy, bronchodilators, relieve hemo-pneumothorax Treatment of Flail Chest Injury Do not underestimate its seriousness Isolated injury with correctible hypoxia Isolated injury with respiratory failure Manage in ICU with good pain control, restrict fluids, bronchodilators, monitor for ventilation and gas exchange, chest physiotherapy, supplemental oxygen Manage in ICU with endotracheal intubation and assisted ventilation Multiple injuries Manage in ICU with endotracheal intubation and assisted ventilation Chest Wall Injury Fractures and Soft Tissue Injury Acute chest wall pain Chest wall and Lung expansion impaired Effects: poor ventilation and unstable alveoli leads to progressive alveolar collapse Impaired cough and mucociliary system Effects: inability to clear air passages of mucoid bronchial secretions with resultant progressive retention segmental or lobar collapse Chest Wall Injury Fractures and Soft Tissue Injury Acute chest wall pain Cannot breathe deeply Cannot cough well Retention of bronchial secretions Increased work of breathing Retention atelectasis V/Q mismatch hypoxia and fatigue Acute Chest Wall Pain Demands immediate control Must restore ability to breathe well and cough well to protect the lungs against retention atelectasis Oral opiods and NSAIDS Intercostal nerve blocks Epidural analgesia – most effective Watch out for respiratory depression Underlying Lung Parenchymal Injury Lung contusion – “lung bruising” - intra-alveolar bleeding and increased capillary permeability Effects: impaired diffusion hypoxia Surface lung laceration – leakage of air and blood into pleural space Effects: impaired lung expansion hypoxia Deep lung explosive tears – bleeding into cavities, pulmonary hematoma Effects: obstruction of peripheral air passages due to blood clots causing segmental or lobar collapse hypoxia and hemoptysis Increased work of breathing Adverse changes in lung and chest wall compliance reason: injury to the lung and chest wall Impaired inter dependency of lung and chest wall reason: altered pleural pressures Increased airway resistance reason: reduced lung volume, contraction of bronchial smooth muscle, retained secretions and blood clots in the air passages Increased work of breathing Increased metabolic demand Hypoxia Chest wall muscle spasm for splinting rib fractures Respiratory muscle fatigue and oxygen debt Respiratory failure Hemothorax Intra-thoracic Bleeding Low pressure Pulmonary parenchyma Stops with lung expansion Self-limiting High pressure Systemic vessels Arteries – ICA, IMA, Aorta, IA, LSA, LCA Veins – AV, SVC Persistent Hemothorax Radiologic diagnosis CXR and CT scan Insert large bore chest tube – 28F or 32F Measure initial blood loss Monitor drainage for next 3 hours Repeat CXR after tube insertion Hemothorax Bleeding into the pleural space is of two types Low Pressure versus High Pressure Low Pressure Bleeding is from torn lung parenchyma and it stops spontaneously with lung expansion. Self Limiting High Pressure Bleeding is from systemic arteries and veins and it is continuous. Not Self Limiting Massive Hemothorax When is urgent thoracotomy necessary? Initial blood loss is > 1500 mls 8% of body weight is blood volume Persistent bleeding at 300 mls/hour for 3 consecutive hours Large amount of retained blood clots on CXR inspite of adequate chest tube drainage Hemothorax Pleural space can accommodate large amount of free and clotted blood >1.5L Hypotension from loss of circulating volume and tension effect Hypoxia from compressive atelectasis High pressure bleeding Systemic, persistent Low pressure bleeding Pulmonary parenchymal, self-limiting Hemothorax Insert a large bore chest tube # 32F Measure initial blood loss CXR lung expanded, unevacuated clotted blood Monitor for on-going bleeding and recognize lifethreatening situation > 500 ml in 1 hr > 400 ml/hr for 2 hrs > 300 ml/hr for 3 hrs Action: Urgent Thoracotomy to stop bleeding Thoracic Trauma The CXR was taken in the ER of a patient involved in a MVA. He is complaining of severe pain in the right chest and unable to breathe. What does it show? What did it arise from? Why is it life-threatening? What treatment is required? Tension pneumothorax Any closed pneumothorax has the potential to become tension type under the right circumstances – persistent coughing, positive pressure ventilation in ICU, under GA Life-threatening due to combination of Hypoxia – collapsed ipsilateral lung and compressed contralateral lung Hypotension – impaired venous return, low stroke volume, low cardiac output Immediate Treatment is Necessary Pneumothorax TENSION SIMPLE Tension Pneumothorax Treat immediately and do not wait for CXR confirmation Decompress affected pleural space with large gauge needle followed by insertion of intercostal chest tube Tension Pneumothorax is a clinical diagnosis CXR is not needed Remember – in chest injury can get bilateral tension pneumothoraces and tell-tale mediastinal shift will be absent Tension Pneumothorax Pressure in pl. space exceeds ambient press. Causing a net positive intra thoracic pressure. Most commonly caused by PP ventilation May occur in spontaneously breathing patient. Characterized by mediastinal shift, compression of functional lung and decrease in venous return. Question A young 18-year-old man is brought to the ER with closed head injury and blunt chest trauma. He has multiple rib fractures on right side with surgical emphysema, and small traumatic pneumothorax. He is hypoxic and O2 saturation is 82% on supplemental oxygen. Assisted ventilation with positive end-expiratory pressure is initiated and soon thereafter there is sudden occurrence of hypotension. What is the most likely cause of hypotension? Tension Pneumothorax Acute Cardio-Pulmonary Collapse Tension Pneumothorax Air continues to leak from lacerated lung or ruptured bronchus into the pleural space because of high airway pressure – result of coughing or positive pressure ventilation Life-threatening due to combination of Hypotension Hypoxia Treat immediately and do not wait for CXR confirmation First insert large gauge needle and then intercostal chest tube Tension Pneumothorax is a clinical diagnosis Tension Pneumothorax Tension Pneumothorax Combination of hypoxia and hypotension is life-threatening Need immediate decompression by insertion of large bore needle followed by insertion of intercostal chest tube Blunt Thoracic Trauma A young man was involved in a high speed head-on accident with another car. The aortogram performed after CXR indicates a dangerous situation, as arrowed. What is it? What causes it? What treatment is required? What are the clinical and the chest radiographic signs that suggest presence of this injury? Thoracic Aortic Injury Thoracic Aortic Injury Clinical indicators of severe chest injury are Sudden deceleration force Fractures of multiple ribs, scapula, sternum, first rib Suspicious CXR findings Who should be screened for Thoracic Aortic Injury? 1. 2. 3. 4. 5. 6. 1. 2. 3. 4. 1. 2. 3. 4. Patient with an abnormal mediastinal silhouette on CXR: loss or irregularity of aortic knob contour widened superior mediastinum (> 8 cm) depression of left main stem bronchus (> 140 degrees from trachea) lateral tracheal deviation rightward deviation of nasogastric tube Apical cap and/or hemothorax Patient with a significant mechanism of injury (irrespective of CXR appearance) crushed steering wheel ejection from vehicle fall > 5 meters major lateral chest impact Any patient with associated injuries including sternal fracture multiple rib fractures scapular fracture first or second rib fracture(s) Thoracic Aortic Injury Transection of the aorta at the junction of mobile aortic arch and fixed descending aorta Deceleration injury Emergency operation to repair ruptured aorta Rule of 85: 85% of victims die at the site of accident from bleeding, 15% reach hospital alive and if missed 85% will die in the first week, and in 85% the site of injury is just distal to left subclavian artery Thoracic Aortic Injury Can you name 6 radiological features of Thoracic Aortic Injury on plain chest x-ray? Do you know the clinical signs of this injury? Why do 85% die at the site of accident? What percentage of the 15% who reach the hospital alive will die in the next 7 days if missed? What is the site of 85% of this injury and why? Thoracic Aortic Injury 20% of all MVA fatalities 85% dead at the site of accident 85% dead with 1 week 85% of tear at the ligamentum arteriosum Trauma takes its toll “ They often arrive in the middle of the night – when the streets are angry and the dark city terrors stalk innocent prey. Or mangled in highway accidents. Or badly injured in accidents at home or work. They are trauma victims. And most of them won’t live to see the coming of dawn. Chest Trauma: Indications for O.R. Hemothorax 1500 ml Ongoing bleed Persistent shock despite resuscitation Documented or suspected injury to airway or esophagus Impalement Massive Hemothorax Circulation Massive bleeding: loss of >20% circulating blood volume effect: hypotension, impaired oxygen transport, metabolic acidosis and impaired cardiac function Severe cardiac injury: myocardial contusion, valve rupture, septum rupture effect: arrhythmias, acute heart failure Cardiac Tamponade: as little as 150-200 ml bleeding into pericardial space is serious effect: acute hypotension due to impaired venous return Cardiac Tamponade Life-threatening state Beck’s triad Hypotension Raised JVP Small quiet heart Rapid accumulation of 150 to 200 ml of blood in the pericardium can be fatal CXR not diagnostic Urgent pericardiocentesis is necessary Intrapericardial Pressure (mm Hg) Cardiac Tamponade and Chronic Pericardial Effusion Rx-Cardiac Tamponade If pt. stable: subxiphoid pericardial window under G.A. Extraperitoneal via midline incision or transperitoneal at laparatomy. Be prepared for immediate med.sternotomy. If unstable: Lt. Anterolateral Thoracotomy. Minor-pledgeted sutures Major-CP bypass. Survival for simple injury >60% Traumatic Pneumothorax Insert 28F or 32F chest tube and expect lung to expand immediately If you find massive air leak from chest tube question What is the reason? Fault with chest tube insertion Fault with connections or drainage system Large lung laceration Rupture of tracheal-bronchial tree or esophagus Unrecognized penetrating chest wound Action: stop suction, examine chest tube insertion site, examine all connections and drainage bottle, immediate CXR, urgent bronchoscopy for airway injury and if present, urgent operation Thoracic Trauma Clinical shock Neck veins flat Massive Bleeding Neck veins distended Tension pneumothorax Cardiac tamponade Cardiac valve rupture Cardiac septum rupture Systemic air embolism Chest Trauma Pitfalls for the unwary Is there a chest injury which is associated with pelvic fracture? Diaphragmatic Rupture Air - Closed Pneumothorax Encroachment on pleural cavity by air Introduced from outside by injury or operation Following injury to the lung or trachealbronchial tree Spontaneous either primary in the absence of underlying lung disease or secondary to a recognized lung disease Perforation of esophagus Pneumothorax Classification Spontaneous Traumatic Primary Secondary Catamenial Neonatal Chest injury: blunt and penetrating Iatrogenic: FNA, thoracentesis, faulty chest tube removal, perforation of esophagus, CVP line insertion, pacemaker insertion, barotrauma from positive pressure ventilation Diagnostic Dangerous situation If clinical examination confirms presence of pneumothorax and patient has Severe shortness of breath, low BP, tachycardia, and dilated neck veins Tension Pneumothorax. Clinical diagnosis. CXR is not necessary for confirmation. Immediate decompression in ER is necessary Low volume state – low BP, pallor, low hemoglobin, tachycardia Hemo-pneumothorax and immediate resuscitation. CXR is necessary, chest tube insertion in ER, and prepare for thoracotomy. Pneumothorax – Disturbed Physiology and Lung Function Limitation of lung expansion inadequate ventilation, the severity of which will vary with the extent of encroachment and vital capacity of the patient Failure to expand lung fully early will result in formation of fibrinous exudate in the pleural cavity and on lung surface fibrosis which may fix the lung in compressed position and impair function Tension effect - impaired ventilation and venous return to the heart hypoxia and hypotension, a life-threatening state Primary Spontaneous Pneumothorax Tall, thin body habitus Young < 40 yrs 5M:1F Rupture of apical bleb (<1cm) or bulla (>1cm) Bleb forms from rupture of apical sub-pleural distended alveolus collection of air bubble within layers of visceral pleura Bulla forms from tractional emphysema due to apical scarring Secondary Spontaneous Pneumothorax Underlying lung pathology COPD -Emphysema Infections - necrotizing pneumonia, abscess, tuberculosis, pneumocystis carinii pneumonia Lung metastases – subpleural Histiocytosis X Cystic fibrosis Sarcoidosis Collagen disorders – scleroderma, rheumatoid arthritis Lymphangioleiomyomatosis - LAM Clinical Presentation Absence of precipitating factors Emergency Room Sudden onset of pleuritic chest pain Shortness of breath O/E hyperinflated chest, tympanitic chest, absent air entry Clinical Presentation symptoms Acute pleuritic type chest pain Dyspnea – worse particularly if underlying lung disease Hypotension and severe dyspnea indicating life-threatening tension pneumothorax Clinical Presentation - signs Affected hemithorax Hyperinflated Tympanitic Reduced air entry Low blood pressure, cyanosis, mediastinal shift, and dilated neck veins indicating lifethreatening tension quality Radiology Chest X-ray – inspiration and expiration films Size estimation Presence of underlying lung disease Associated hemothorax CT scan chest in recurrent pneumothoraces Management Observation Mild symptoms No progression Size is small: <20%, <4cm from apex, <1cm from chest wall expect spontaneous resolution at rate of 1.25%/day Intercostal chest tube drainage Size is large: >20%, >4cm from apex, >1cm from chest wall Tension quality Progression noted Undergoing general anesthesia Goal is to relieve symptoms and permit early full re-expansion of lung Results Early 5-10% will require surgical intervention because of prolonged air leak beyond 3 days Long term with conservative treatment recurrence after 1st episode 15-20%*, after 2nd episode 40 50%, after 3rd episode 80% * usually within 2 years, 75% ipsilateral Indications for chest tube insertion in Pneumothorax Large size at initial presentation Increasing size Symptomatic Associated hemothorax Undergoing general anesthesia Bilateral Tension quality Contralateral Indication for Surgery First episode with prolonged air leak > 3 days 2nd or 3rd recurrence on same side 1st occurrence on contra-lateral side Associated hemothorax >1000mls Associated pleural sepsis Incomplete re-expansion Occupational risks Synchronous bilateral Life-threatening episode Patient living in remote areas Therapeutic Options Apical bullectomy and parietal pleurectomy Video-assisted thoracoscopic approach Limited thoracotomy Chemical pleurodesis - elderly Talc Tetracycline Traumatic Pneumothorax Barotrauma from positive pressure ventilation Insertion of central venous lines, pacemaker leads Cervical lymph node biopsy Percutaneous and transbronchial lung biopsy Perforated esophagus – post-emetic or instrumental Chest injury with rib fracture causing lung laceration or tracheal-bronchial tear