to review the presentation. - The Chicago Metropolitan Trauma Society
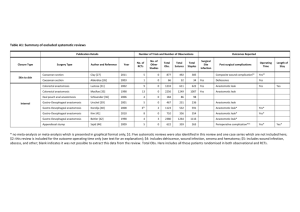
advertisement

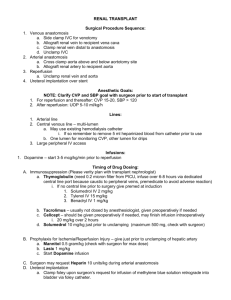
Chicago Metropolitan Trauma Society 4/15/2015 • Discussion objectives – Management of penetrating renovascular trauma – Colonic anastomosis after damage control laparotomy – Is it worth the risk? – Anticoagulation management strategies after IVC injuries requiring ligation of IVC. Traumatic Colon Injury and Open Abdomen – Is anastomosis worth the risk? Greg Day MD Loyola University Medical Center Patient - CC • Presentation – 22 y/o Male s/p stab to the left flank – Primary Survey • Airway – intact, shallow respirations • Breathing – Bilateral breath sounds • Circulation – tachycardic 120s, hypotensive to 70’s, weakly palpable femoral pulses bilaterally Patient CC • Secondary Survey – Pertinent findings • Neuro – Awake, alert, responsive to questions – c/o abd pain • Abd – Left flank stab approx 3cm in length, active bleeding from site, digital probe beyond fascia • No other injuries noted • Resuscitation – CVC placed – Massive transfusion protocol activated – First units of blood transfusing while going to OR Operative and Hospital Course • Operative Findings – Large hemoperitoneum, Grade V injury to left renal hilum. Descending colon injury >50% circumference. – Colon resected, left in discontinuity – Left nephrectomy performed. – Procedure complicated by cardiac arrest • ACLS x20 minutes – ROSC – Abdomen packed, abthera placed and patient to ICU for resuscitation Resuscitation • In OR – 3L IVF, 12u PRBCs, 13u FFP, 2 Plt • ICU Care – Hypoxemia resolved over next 24-36 hours – Vasopressors weaned off – Acidosis resolved, base deficit cleared Hospital Course • Return to OR POD 2 for abdominal washout, primary colonic anastomosis and replacement of vac • POD 5 – return to OR for fascial closure • POD 8 – Patient with stool from midline wound – return to OR for resection of anastomosis, end colostomy • Patient Discharged to home three weeks from injury • Stoma reversed successfully 6 months later Prior to Colonic Anastomosis • Pt Base deficit had cleared • Vasopressors were off • Transfusion requirements post op were minimal • Bowel appeared viable • Why was it not successful? Colonic Anastomosis in Trauma Colon Anastomosis in Trauma • 1979 Stone/Fabian found that in the stable patient, primary repair can be performed safely at initial operation without diversion • This was subsequently confirmed with following studies with primary anastomosis also Seeing good results • How then does the open Abdomen affect your ability to perform an anastomosis? Damage Control Laparotomy • “Damage Control” – Procedures and skills used to maintain/restore the watertight integrity, stability or offensive power of a warship. • Damage Control Surgery – limit surgery to essential interventions – Control hemorrhage, limit enteric contamination • Decision to perform damage control – Clinical decision – Objective signs • • • • Temp < 35C pH <7.2 Base Deficit - > 15mmol/L INR > 50% of normal When is anastomosis appropriate? • Difficult to study prospectively • Most data at this time is retrospective in nature • Why risk it? – Repeat operations incur high risk - 78 Damage Control Laparotomy with colon injury – 61 analyzed - Findings - 16% leak rate of those patients receiving anastomosis - In comparison to 1-3% leak rate in non damage control surgery - Leaks – longer ICU stay, decreased likelihood of fascial closure - Risks for Leaks - Older Age Failure to close fascia in five days - This study also had 2/10 leaks in a defunctionalized anastomosis - Question then – does proximal diversion help in trauma setting? - Anastomotic breakdown is suggested to be more related to physiology of severe injury • 68 Patients with DCS with colonic injury – 41 with anastomosis, 27 diverted • Leak = suture line disruption or EC fistula – Leak rate – DCS compared to Non-DCS • 17%-6% – When comparing leak vs no leak • No difference in transfusion requirement, anastomosis technique – They did find significant difference in leak rate in those patients with vasopressor use between DC and operation when anastomosis was performed Colon Anastomosis After Damage Control Laparotomy: Recommendations From 174 Trauma Colectomies Ott, Mickey M. MD; Norris, Patrick R. PhD; Diaz, Jose J. MD; Collier, Bryan R. DO; Jenkins, Judith M. MSN; Gunter, Oliver L. MD; Morris, John A. Jr. MD • Goal to compare leak rates between open abd pts and those primarily closed at first operation • 174 patients with DCS with colonic injury – 58 with fecal diversion, 116 with colonic anastomosis Colon Anastomosis After Damage Control Laparotomy: Recommendations From 174 Trauma Colectomies Ott, Mickey M. MD; Norris, Patrick R. PhD; Diaz, Jose J. MD; Collier, Bryan R. DO; Jenkins, Judith M. MSN; Gunter, Oliver L. MD; Morris, John A. Jr. MD How should we proceed? • Trauma patients who require damage control operations are under more physiologic stress • Markers of transfusion requirements, acidosis, temperature, and vasopressor requirements are surrogates to prove their stressed state • It is these factors one must consider when discussion anastomosis after a patient has an open abdomen How has the literature helped • Patients with massive transfusion requirements, left sided colon injuries and vasopressor requirements should most often be diverted • Consideration of anastomosis beyond those factors remains a clinical judgment call. Anticoagulation management after IVC ligation Harold Bach MD Loyola University Medical Center AB 2767036 • 22 y/o male involved in altercation at a bar • Sustained GSW to abdomen, mid-epigastric region • Unstable at OSH (Level II trauma center), so taken immediately to OR • Liver injury attempted to be repaired AB 2767036 • Upon arrival to trauma bay, patient intubated and sedated • PRBC transfusing • HR 115 BP 140 systolic • Abdomen open and packed • Taken back to OR for exploration AB 2767036 • At OR, diagnosed injuries included: – shredded IVC, – multiple areas of bleeding from IVC side branches and side branches of aorta, – aorta without obvious injuries, – injury to lumbar vertebral body, – supraceliac aortic clamping time 50 minutes. AB 2767036 • Procedures included: – Damage Control Exploratory laparotomy, – ligation of infrarenal IVC, – packing of liver with Vicryl mesh, – packing of abdomen, – Abdomen left open with Bogota closure • Taken back to ICU for resuscitation AB 2767036 • Stabilized, taken back to OR PID #2 – Found to additionally have a pancreatic head injury and small bowel serosal injury – Reexploration of recent laparotomy, – removal of packing, – abdominal washout, – placement of drains to retroperitoneum, – abthera vac placement AB 2767036 • Returned to OR 2x more, eventually closed with feeding jejunostomy tube placed • Post op course complicated by patient selfdiscontinuing retroperitoneal drains requiring IR replacement • Began on coumadin, discharged home Abdominal IVC injuries • Incidence – Penetrating 0.5-5% – Blunt 0.6-1% • Mortality – 19%-66% in literature, widely reported around 40% • Rx: – Lateral venorrhaphy • Patient stable • Technically feasible • Must have >25% luminal diameter remaining – IVC ligation • Damage control • The first report of an IVC ligation was by Kocher (1883). • Bilroth performed the procedure in 1885. – These were for iatrogenic injuries to during surgery for malignant disorders in two patients. – Both of these patients demised. • The first record of an infrarenal vena caval ligation with a successful outcome was by Bottini. • Detrie reported the first survivor after a suprarenal ligation. • By 1949 there were 136 reports of caval ligations in the literature. • DeBakey et al reported the first large series of AVC injuries in 1978. – 301 patients who had been identified with caval injuries / 30 years. – The majority (234) were treated with repair while only 32 received caval ligation. – Initial mortality rates in the 1950’s approached 100%. • It was also historically a procedure employed to halt the propogation of LE DVT prior to anticoagulation therapy. Sequelae of IVC ligation • In repaired IVC, recommend surveillance via US or CT • Ligated IVC? • Anticoagulation? • Role of prophylactic fasciotomies? Questions: • What are the EAST guidelines on treatment with anticoagulation after ligation of the infrarenal IVC? • A) 3 months therapeutic anticoagulation • B) 6 months therapeutic anticoagulation • C) lifetime anticoagulation • D) there are no guidelines for treatment Answer - D Question • Current guidelines suggest that patients with a destructive colon injury can undergo resection and primary anastomosis if • A – There is no evidence of shock • B – Minimal underlying disease • C – Minimal associated injuries • D – There is no peritonitis • E – All the above are present Answer - E Question • True/False : In penetrating renovascular trauma, preliminary vascular control decreases blood transfusions, decreases rate of nephrectomy and decreases blood loss. Answer – False – Preliminary vascular Control has no impact on the above.