Document
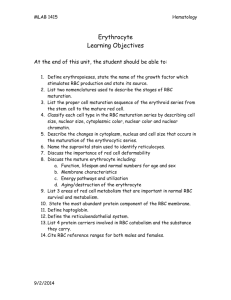
advertisement
RED BLOOD CELL FORMATION Dr. B.L. Mtinangi. Department of Physiology HKMU November, 2015 1 RED BLOOD CELL FORMATION Rbc’s are circular, biconcave, disk-like, dumbbell shaped, non nucleated living cell. Mean Cell Volume (MCV) is the average volume of each red cell (82-92cub micron) Mean Cell Haemoglobin (MCH) is the average Hb in each cell (27-32 picogram) Mean Cell Haemoglobin Concentration (MCHC) this indicates the degree of saturation of Rbc with Hb (32 to 38%) RBC’s CONT. During Anaemia MCHC is less, it is known as hypochromic anaemia and If MCHC is normal it is normochromic anaemia Biconcave shape gives certain advantages: Maximum surface area for gas diffusion Diffusion distance is minimised Rbc can mould their shape while passing through narrow capillaries 3 RBC’s FORMATION There is some daily loss of Rbc’s ie the average life span of Rbc’s is about 120 days To keep the Rbc’s count normal or to balance this loss Sufficient number of Rbc’s must be produced daily 4 FORMATION OF Rbc Formation/generation (ERYTHROPOIESIS) starts in the third week of INTRAUTERINE life. Third week to third month erythropoiesis occurs in the mesoderm of the york sac Third month to fifth month it occurs in the liver and spleen (HEPATIC PHASE) Fifth month onwards it occurs in the red bone marrow 5 HAEMATOPOIESIS 6 FORMATION OF Rbc CONT. Post natal (after birth) red blood cell formation (erythropoiesis) occur in the RED BONE MARROW Main sites for erythropoiesis: Ribs, vertebra, sternum, cranium Pelvis. Shaft of the femur and tibia 7 BLOOD FORMING TISSUES Myeloid tissues produces Rbc,Wbc and Platelets. Lymphoid tissues include the lymph node, thymus and spleen. All produce Lymphocytes 8 RBC maturation 10 Rbc DEVELOPMENTAL STAGES Pluripotent stem cell ( Uncommitted stem cell) develop into Committed stem cell into Pronormoblast or Myeloblast or Megaloblst or Lymphoblast Pronormoblast (Proerythroblast) develop into Early normoblast then to Intermidiate normoblast then to Late normoblast then into immature Rbc (Reticulocyte) then within 2 to 3 days develop into mature Rbc 11 FORMATION OF Rbc CONT. One committed stem cell produces 16 mature Rbc1 10% to 15% of Rbc undergo premature destruction during development 12 NORMAL VALUES Total normal Rbc count: men 4.5 to 6.4 mill/cumm women 3.9 to 5.6 mill/cumm Normal Haemoglobin (Hb) concentration: men 13 to 17g/dl women 11 to 16g/dl 13 FACTORS INFLUENCING ERYTHROPOIESIS 1. Erythropoietin. Is a hormone produced in JuxtaGlomerular Apparatus(JGA) in the macula densa (kidney) Is a glycoprotein with MW 36000 Stimulate proliferation and differentiation of erythroblast Stimulate Hb synthesis Promote Rbc maturation 14 2. VITAMINS VITAMIN B12 Is essential for erythropoiesis ie it stimulates erythropoiesis Present only in meat, fish and diary products Absent in vegetables In the GIT it combines with the intrinsic factor which protect & transport it to the terminal ileum Absorbed in the terminal ILEUM Required for DNA and RNA SYNTHESIS 15 3. FOLIC ACID Folic acid is another vitamin that is essential Stimulates erythropoiesis Required for DNA and RNA synthesis Present in vegetables and fruits 16 4.IRON IRON: Found in the meat and vegetable Required for Haemoglobin synthesis Daily intake is about 10 to 20 mg 5% to 10% of iron daily intake is absorbed ie (0.5 to 2mg/day) 2/3 of Iron is found in the Rbc It circulate in the blood as Transferrin Stored in the bone as Ferritin and Haemosiderin 17 Red Blood Cell Turnover A summary of: Bilirubin formation, circulation and elimination Senescent (old) Red blood cell destruction Hb is degraded to Haem & Globin Globin is reutilised as Amino Acid Haem an Iron component is degraded to a porphyrin ring Porphyrin ring is converted to choleglobin CONT Choleglobin in the presence of an enzyme haem oxygenase is converted to BILIVERDIN Biliverdin in the presence of an enzyme biliverdin reductase is converted to BILIRUBIN Bilirubin is released into plasma CONT In the plasma Bilirubin is bound to ALBUMIN and transported to the liver In the liver bilirubin is conjugated with GLUCURONIC ACID to conjugated bilirubin (bilirubin glucuronide) CONT. Conjugated bilirubin is transported to the intestine through the bile duct In the intestine bilirubin is further conjugated by the bacteria to STERCOBILINOGEN Stercobilinogen is oxidized to stercobilin after exposure to air in the feces CONT The reminder 5% is absorbed (enterohepatic circulation) and transported to the kidney as UROBILINOGEN Urobilinogen is oxidized to UROBILIN after exposure to air in the urine ANAEMIA Anaemia is defined as the reduction of: Haemoglobin Total red cell count Haematocrit (Packed cell volume – PCV) According to age and sex 25 CAUSES OF ANAEMIA Causes could be due to: Nutritional deficiences, eg iron, folic acid, vitamin B12 ect ects Excessive destruction of Rbc eg due to malaria, sickle cell disease etc etc External/ internal bleeding Infestations eg hookworm Bone marrow failure 26 Thank you