Bariatric Surgery
advertisement
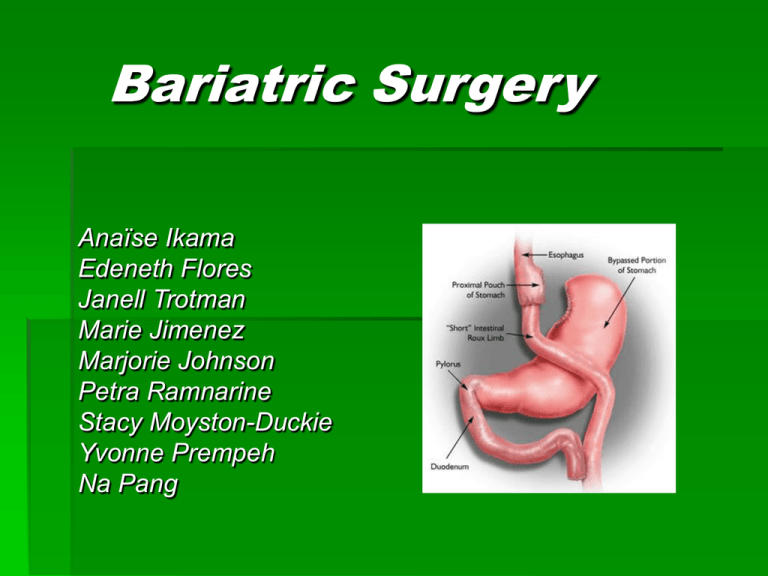
Bariatric Surgery Anaïse Ikama Edeneth Flores Janell Trotman Marie Jimenez Marjorie Johnson Petra Ramnarine Stacy Moyston-Duckie Yvonne Prempeh Na Pang What is Bariatric Surgery by Yvonne Prempeh What is bariatric surgery? Bariatric surgery is the term for operations to help promote weight loss. There are three types of bariatric surgery: LAP- BAND® system, Vertical Banded Gastroplasty(VBD), & Roux-en-Y Gastric Bypass LAP – BAND® SYSTEM An adjustable silicone elastic band is placed around the upper part of the stomach creating a small pouch and restricting the passage of food VERTICAL BANDED GASTROPLASTY (VBG) VBG is a purely restrictive procedure in which the upper stomach is stapled and divided, forming a small pouch that reduces the size of the stomach and the amount of food the stomach can hold ROUX-EN-Y GASTRIC BYPASS Roux-en-Y Gastric Bypass is the most frequently performed weight loss procedure in the United States During this surgery, the upper stomach is stapled creating a small pouch that is completely divided from the remainder of the stomach Requirements for Bariatric surgery by Petra Ramnarine Criteria before surgery BMI of 40+ 80 - 100lbs overweight Diabetes, heart disease or severe apnea Related physical problems that significantly employment, physical mobility or physical function Criteria for insurance companies Obtaining approval can take up to 4 weeks from insurance company Pt will be responsible for out of pocket fees as outlined in policies Nutrition: Diet plan for Bariatric Surgery by Janell Trotman Nutrition Patient have to follow a strict diet before and after bariatric surgery. Patient must have a nutritional consultation. Pre-Post Operative Nutrition Clients are started on a puree or liquid diet 2 weeks before surgery. Most of the caloric intake should contain mostly of protein. Caffeine, soda, alcoholic and beverages that contain sugar should be avoided. Food Restriction It is important to chew food thoroughly and slow It is important wait 2-3 minutes after swallowing before putting the next bite of food in your mouth. Don’t drink fluids while eating Food Restrictions Avoid food high in fat and have no nutritional value. Food Restriction Avoid alcohol Avoid food high in sugar Limit snacking between meals Pre-operative Nursing Care By Marjorie Johnson Pre-operative Nursing Care There are always risks with surgery, however as health care providers, we can follow steps to minimize these risks by performing physical and psychosocial assessment of the patient. The psychosocial assessment is obtained to evaluate the patient’s mood, self-esteem and emotional status. Some of the complications for bariatric surgery DVT, pulmonary Embolus, pneumonia, dumping syndrome, loss of too much weight, injury to pelvic organ, and leaks from a break in the staple line, and death (1% nationwide). Sign Consent The patient has the right to be informed of the tests, treatments, or procedures, therefore, should be asked to sign consent; a legal piece of paper that tells exactly what will be done to the patient. Forms that gives caregivers permission to certain tests, treatments, or procedures. If unable to give his/her consent, someone who has permission could sign the form instead. Special Equipments With bariatric surgery patient, special equipments have to be ordered and explained to patients. Post-operative Nursing Care By Stacy Moyston-Duckie Complications developed after Bariatric surgery Bariatric-surgery patients are at risk for developing complications related to surgery and postoperative respiratory and gastrointestinal disorders. According to the International Bariatric surgery registry, the leading cause of death following bariatric surgery is pulmonary embolism, anastomotic leaks and respiratory failure. Other complications are wound infections, incisional hernias, ulcers, bleeding, constipation, cholelithiasis, dumping syndrome, dehiscence, vitamin and nutrient deficiencies. The role of the nurse in monitoring and managing clients in postoperative Typically, during the postoperative recovery period the nurse has to monitor and manage the patient to reduce complications, by positioning the patients head at least 30 degrees semi-fowler’s position to help breathing and by reducing the weight of abdominal adipose tissue pressing on the diaphragm. Checking vital signs, assess for complications, and provide skin and wound care, breathing exercises using incentive spirometry. Assess abdominal changes in appearance of volume gastric or percutaneous drains, presence of hematemesis or melena, and persistent cough. These findings should be reported to the physician for appropriate medical intervention. (www.aafp.org). Also encourage early ambulation to reduce the risk of immobility. Pain Medications Post-operative pain medications are given through ‘patient controlled analgesia’ (PCA) pump, which dispenses (morphine) when the patient pushes a button. They patient will also receive IV injections of Torodol. Torodol is similar to Motrin and helps relieve abdominal muscle pain. After day two surgery the patient’s medication will be switched from PCA machine to a liquid medicine Roxicet – liquid Percocet that will be taken by mouth every 4-6 hours. Appetite suppressant medications Appetite suppressants medications are given such as Phentermine (Adepex-P, and Obsestin-30) which acts directly on the appetite-control center in the CNS to suppress and reduce hunger. Sibutramine (Meridia), also reduces hunger and increases sensations of satiety by inhibiting the uptake of serotonin, norepinephrine, and dopamine Ursodiol, this drug is to taken twice a day, two weeks after surgery. Actigall is taken to prevent gallstones from forming during rapid weight loss. Patients who have done bariatric surgery will need to take vitamin and mineral supplement for the rest of their lives. Preventive Measures Against Obesity •Diet •Exercise •Group support by Na Pang Exercise Exercise plays a crucial role after bariatric surgery because Promotes good circulation, respiration Increases metabolism, reduces adipose tissues How to start an effective exercise pattern Walking is the simple way to start the exercise process Then, try out different types of exercises to find one that is enjoyable, running, treadmill. However, exercises should be well-organized. Ongoing Support Study shows that Support groups, one of the best things, after bariatric surgery, keep the weight off. Rationale Surgery requires lifestyle and behavioral changes, patients need the support of family, friends, and healthcare professionals to help them get through any rough spots. Nursing Care Plans for Bariatric Surgery by Marie Jimenez, SPN Nursing Care plans: Bariatric Surgery Pre-operative Nursing Diagnosis: Disturbed Self-Concept Post-operative Nursing Diagnosis: Ineffective Breathing Pattern For patients undergoing bariatric surgery, it is important to note that there are nursing care plans designated for the preoperative and postoperative phase. Pre-op Nursing Diagnosis: Disturbed Self-Concept related to obesity & inability to lose weight by conventional methods Nursing Outcome Nursing Intervention Client will demonstrate 1. positive self-concept AEB Verbalizing feelings Positive statements Active participation in self-care 2. 3. Assess for signs and symptoms of a disturbed selfconcept Implement measures to assist client to increase self-esteem Measures for client to adapt to body changes Nursing Rationale 1. 2. 3. Recognition allows for prompt intervention An increase in self-esteem has a positive effect on client Impact of changes in selfconcept Post-op Nursing Diagnosis: Ineffective Breathing Pattern r/t increased RR associated with fear/anxiety & decreased RR associated with depressant effect of anesthesia Nursing Outcome Nursing Intervention 1. Assess for Signs & Sx of an ineffective breathing pattern 1. 2. Monitor for i in 2. Client will maintain clear open airways oximetry results AEB 3. Normal breath sounds Normal rate & depth of respirations Absence of dyspnea Nursing Rationale 4. Place client in semi- to high fowlers position Instruct clients to use incentive spirometer q 1-2 h 3. 4. Recognition allows for prompt intervention Assist in evaluating respiratory status Allows for max. diaphragm excursion Promotes max. inhalation & lung expansion Assessment provides vital clues regarding how nursing care affects the psychosocial aspect of the patient Therapeutic communication encourages self-awareness Nurses should be aware of protocols when deviations of breathing patterns occur for proper interventions to take place Any signs of respiratory distress should be reported and documented immediately Discharge/Client teaching by Anaise E Ikama Discharge/Client teaching Medications: analgesics for pain, anti-emetics to prevent dehydration and vitamins to ensure adequate intake of nutrition Wound care should be taught to prevent infections Activity progression any abdominal exercises, weight Lifting or swimming should not be attempted. Ambulate to prevent DVT Diet: eat small meals due to the small size of the stomach Discharge/Client teaching Report symptoms: To the ER Issues that require urgent medical attention, such as: chest pain, shortness of breath and excessive abdominal pain Contact the physician For non-emergent issues such as: nausea, vomiting, diarrhea or fever, redness, swelling, drainage or bleeding from the incision Discharge and Client Teaching by Edeneth Flores D/C and Client teaching: Instruct patients to take their prescribed medications. Some of the medications are: Analgesics ( pain) Anti-emetics (prevent dehydration) Vitamins ( to maintain the nutrition of the patient) D/C and Client teaching: Teach wound care: Teach about the S/S of infection: Redness Swelling Pus/abnormal discharge from the incision site Pain Difficulty breathing Vomiting Fever Epigastric pain CALL MD if 2 or more of these symptoms persist: D/C and Client teaching: NUTRITION Eat small snack due to small capacity of the stomach. Chew food slowly and cut into pieces. If able to tolerate liquids, the surgeon will likely to recommend having a puree diet, then begin eating 3 meals per day. Eat a few tablespoons at a time to prevent the stretching of the incision site. Eat a few tablespoons at a time to prevent the stretching of the incision site Includes protein to promote healing. D/C and Client teaching: Avoid heavy lifting Encourage ambulation and leg exercises Emphasize the importance of Follow-up visits; patients condition Support groups