Physiology Ch. 42 p515-523 [4-25
advertisement
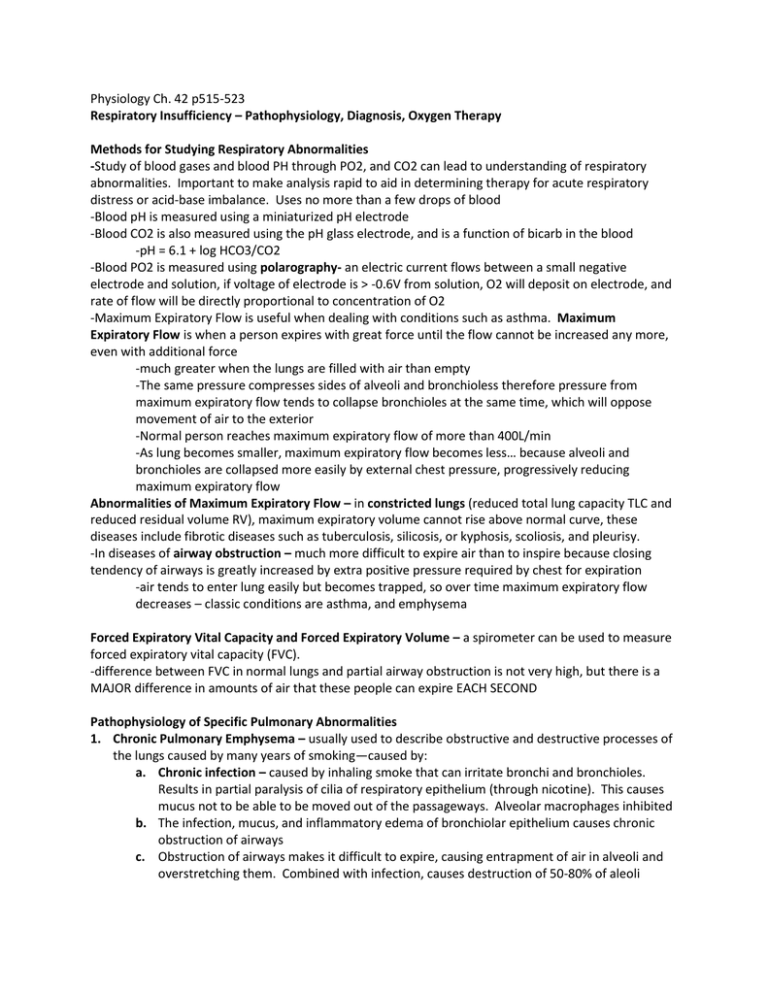
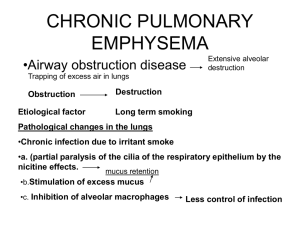
Physiology Ch. 42 p515-523 Respiratory Insufficiency – Pathophysiology, Diagnosis, Oxygen Therapy Methods for Studying Respiratory Abnormalities -Study of blood gases and blood PH through PO2, and CO2 can lead to understanding of respiratory abnormalities. Important to make analysis rapid to aid in determining therapy for acute respiratory distress or acid-base imbalance. Uses no more than a few drops of blood -Blood pH is measured using a miniaturized pH electrode -Blood CO2 is also measured using the pH glass electrode, and is a function of bicarb in the blood -pH = 6.1 + log HCO3/CO2 -Blood PO2 is measured using polarography- an electric current flows between a small negative electrode and solution, if voltage of electrode is > -0.6V from solution, O2 will deposit on electrode, and rate of flow will be directly proportional to concentration of O2 -Maximum Expiratory Flow is useful when dealing with conditions such as asthma. Maximum Expiratory Flow is when a person expires with great force until the flow cannot be increased any more, even with additional force -much greater when the lungs are filled with air than empty -The same pressure compresses sides of alveoli and bronchioless therefore pressure from maximum expiratory flow tends to collapse bronchioles at the same time, which will oppose movement of air to the exterior -Normal person reaches maximum expiratory flow of more than 400L/min -As lung becomes smaller, maximum expiratory flow becomes less… because alveoli and bronchioles are collapsed more easily by external chest pressure, progressively reducing maximum expiratory flow Abnormalities of Maximum Expiratory Flow – in constricted lungs (reduced total lung capacity TLC and reduced residual volume RV), maximum expiratory volume cannot rise above normal curve, these diseases include fibrotic diseases such as tuberculosis, silicosis, or kyphosis, scoliosis, and pleurisy. -In diseases of airway obstruction – much more difficult to expire air than to inspire because closing tendency of airways is greatly increased by extra positive pressure required by chest for expiration -air tends to enter lung easily but becomes trapped, so over time maximum expiratory flow decreases – classic conditions are asthma, and emphysema Forced Expiratory Vital Capacity and Forced Expiratory Volume – a spirometer can be used to measure forced expiratory vital capacity (FVC). -difference between FVC in normal lungs and partial airway obstruction is not very high, but there is a MAJOR difference in amounts of air that these people can expire EACH SECOND Pathophysiology of Specific Pulmonary Abnormalities 1. Chronic Pulmonary Emphysema – usually used to describe obstructive and destructive processes of the lungs caused by many years of smoking—caused by: a. Chronic infection – caused by inhaling smoke that can irritate bronchi and bronchioles. Results in partial paralysis of cilia of respiratory epithelium (through nicotine). This causes mucus not to be able to be moved out of the passageways. Alveolar macrophages inhibited b. The infection, mucus, and inflammatory edema of bronchiolar epithelium causes chronic obstruction of airways c. Obstruction of airways makes it difficult to expire, causing entrapment of air in alveoli and overstretching them. Combined with infection, causes destruction of 50-80% of aleoli -physiologic effects of emphysema are variable depending on severity of disease and degree of obstruction vs parenchymal destruction. Among the abnormalities: A. Bronchiolar obstruction increases airway resistance and results in greatly increased work of breathing B. Loss of alveolar walls greatly decreases diffusing capacity of lung = less oxygenating C. Worse in some parts of the lung compared to others, so some well ventilated and others aren’t. Causes abnormal ventilation-perfusion ratios D. Loss of alveolar walls also decreases pulmonary capillaries through which blood can pass, causing pulmonary hypertension -emphysema progresses slowly over many years, person develops hypoxia and hypercapnia because of hypoventilation and loss of alveolar walls, causing Air Hunger until death 2. Pneumonia – includes any inflammatory condition of the lung in which some or all alveoli are filled with fluid and blood cells. Common type is bacterial pneumonia caused by pneumococci -begins with infection in alveoli, pulmonary membrane becomes inflamed and porous so fluid and white blood cells leak out of blood into alveoli. -infection spreads from alveolus to alveolus, and entire lobes become consolidated (filled with blood) -gas exchange functions of the lungs decline in different stages of the disease -early stages: localized to one lung with alveolar ventilation reduced but blood flow normal -reduces total surface area for respiration and decreases ventilation-perfusion ratio— both of which cause hypoxemia and hypercapnia (high blood CO2) 3. Atelectasis – collapse of the alveoli in localized or entire lung, caused by total obstruction of airway or lack of surfactant in fluids lining alveoli a. Airway Obstruction Causes Lung Collapse – results from blockage of many small bronchi with mucus, or obstruction of major bronchus by large mucus plug (such as tumor) i. can create negative pressures which can cause filling of alveoli with fluid which can cause massive lung collapse ii. collapse of lung tissue not only occludes alveoli but also increases resistance to blood flow, and hypoxia further constricts vessels iii. Vascular constriction causes reduced blood flow to atelectatic lung b. Lack of surfactant as a cause of lung collapse – surfactant is secreted by special alveolar epithelial cells into fluids that coat inside surface of lung to decrease surface tension i. In hyaline membrane disease (respiratory distress syndrome) in newborns, quantity of surfactant is depressed such that surface tension becomes increased, collapsing lungs and causes suffocation 4. Asthma – caused by spastic contraction of smooth muscle in bronchioles causing obstruction a. Cause is usually contractile hypersensitivity in response to foreign substances (allergy). In older people it is usually non-allergens such as smog b. Allergic reaction happens due to many IgE antibodies formed on mast cells in the lung interstitium in close association with bronchioles and small bronchi i. Allergen reacts with IgE to cause mast cells to release histamine, slow reacting substance of anaphylaxis, eosinophilic chemotactic factor, and bradykinin. ii. Combined efforts of these are to produce localized edema of small bronchioles and secrete thick mucus into bronchiolar lumens and spasm of smooth muscle which increases airway resistance iii. Bronchiolar diameter is reduced during expiration in asthma caused by collapse during expiratory effort. Because bronchioles are already occluded in asthmatic lungs, further occlusion from external pressure creates severe obstruction. iv. Reduced maximum expiratory rate and reduced timed expiratory volume, causes dyspnea or air hunger v. Functional residual capacity and residual volume of lung become increased during acute asthmatic attack because of difficulty expiring air from lungs, over years chest cage enlarges causing barrel chest 5. Tuberculosis – tubercle baccili cause reactions in the lungs including invasion of tissue by macrophages and “walling off” of the lesion by fibrous tissue to form the tubercle. a. Walling off helps limit further transmission of tubercle bacilli in lungs and is protective b. In 3% of untreated TB, walling off fails and tubercle bacilli spreads to entire lungs c. In late stages of TB, characterized by fibrosis throughout lungs as well as reduced total amount of functional lung tissue i. Cause increased work on respiratory muscles, reduced total respiratory surface area, diminished pulmonary diffusing capacity, abnormal ventilation-perfusion ratio Hypoxia and Oxygen Therapy – There are various kinds of hypoxia that may/may not need O2 therapy 1. Inadequate oxygenation of blood in lungs due to low O2 in atmosphere or hypoventilation 2. Pulmonary disease- hypoventilation (airway resistance), abnormal perfusion or diffusion 3. Venous-to-arterial shunts 4. Inadequate O2 transport to tissues by blood – anemia/abnormal hemoglobin, circulation deficit, tissue edema 5. Inadequate tissue capability of using O2 – poisoning of oxidation enzymes, diminished metabolic activity a. Cyanide poisoning causes block of cytochrome oxidase to such an extent that tissues cannot use O2 even when plenty is available b. Deficiencies of tissue cellular oxidative enzymes or other elements can lead to this hypoxia, such as those caused by Beriberi, in which several important steps in tissue utilization of O2 and formation of CO2 is compromised because of vitamin B deficiency Effects of Hypoxia on the Body – causes death of cells throughout body, or can depress mental activity (coma), and reduces work capacity of muscles O2 Therapy in Different Types of Hypoxia – O2 can be administered by placing patient’s head in a tent containing O2, allowing patient to breathe pure O2 from a mask, or intranasal tube O2. -in atmospheric hypoxia, providing O2 is 100% effective -in hypoventilation hypoxia, person breathing 100% O2 can move 5x as much O2 into alveoli with each breath and can be beneficial -in hypoxia caused by impaired alveolar membrane diffusion, 100% O2 can increase PO2 in lung alveoli to increase gradient for diffusion, can be effective -hypoxia caused by anemia, abnormal Hgb transport, circulatory deficiency, or physiologic shunt, O2 therapy is much less valuable because normal O2 is already available -in different types of hypoxia caused by inadequate tissue use of O2, O2 delivery is not beneficial Cyanosis – means blueness of skin, cause is excessive amounts of deoxygenated hemoglobin skin capillaries. General cyanosis occurs whenever arterial blood contains more than 5 grams deoxygenated blood in each 100mL of blood. -Anemic person never becomes cyanotic because there isn’t enough hemoglobin for this to occur -In Polycythemia Vera (excess red blood cells) causes frequent cyanosis under normal conditions Hypercapnia – Excess CO2 in body Fluids – only occurs with hypoxia during hypoventilation or circulatory deficiency -hypoxia caused by too little O2 in air, too little Hgb, or poisoning of oxidative enzymes has only to do with availability of O2 or its use, therefore hypercapnia is not concomitant of these types of hypoxia -in hypoxia resulting from poor diffusion through pulmonary membrane or through tissues, serious hypercapnia can occur which stimulates pulmonary ventilation, correcting hypercapnia but not hypoxia -Hypoxia caused by hypoventilation is when CO2 transfer between alveoli and atmosphere is affected as much as is O2 transfer, Hypercapnia DOES occur here -in circulatory deficiency, diminished flow of blood decreases CO2 removal resulting in hypercapnia in addition to hypoxia -When alveolar PCO2 rises above 60-75mmHg, air hunger in normal person can become severe -if PCO2 rises above 80-100mmHg, person becomes lethargic and even comatose -PCO2 of 120-150 causes anesthesia and death, depressing respiration and causing more CO2 buildup. Dyspnea – mental anguish associated with inability to ventilate enough to satisfy demand for air, synonym is air hunger. Three factors associated with development of sensation: 1. Abnormality of gases in body fluids 2. Amount of work that must be performed by respiratory muscles for ventilation 3. State of mind (neurogenic or emotional dyspnea) -A person becomes dyspneic from excess buildup of CO2 in body fluids. However, if levels of CO2 and O2 are normal due to forceful breathing, the activity of respiratory muscles gives person sensation of dyspnea Artificial Respiration 1. Resuscitator – tank of O2 or air, mechanism for applying positive pressure and negative pressure, and a mask that fits over the face of a patient or connector for endotracheal tube. 2. Tank Respirator – Iron lung, patient’s body inside tank and head protruding through flexible but airtight collar, positive pressure develops around body to cause expiration, negative pressure causes inspiration Effect of Resuscitator and Tank Respirator on Venous Return – pressure inside lungs becomes greater than pressure everywhere else in body when using these machines. Flow of blood into the chest and heart from peripheral veins becomes impeded, which can reduce cardiac output to lethal levels