Discuss the reasons why patients and residents
develop pressure ulcers
Discuss implications of patient disease process
at end of life such as: anxiety, anger;
depression, and how this processes impact
CNA care modalities
Incorporate preventive/intervention measures
into one’s role as a CNA
Age
Lack of mobility
Poor diet
Moisture
Mental, neurological and other physical disease
processes
Friction and shearing
Bed sheets and chairs with wrinkled sheet or
hard objects
Previous hx of pressure ulcers
1st warning sign:
› Pink skin on bony prominence that turns white
(blanching)
Further progresses to red/irritated
area…may be warm to the touch…patient
may feel “burning” sensation at ulcer site
Top layers of the skin will break
down/away…becoming an “open sore” which
may exposure bone, muscle or joint
Prevent skin breakdown and discomfort
through proper positioning in bed
Thoroughly clean patient after any soiling
Apply moisturizing lotion as directed by
nurse
Place padding between knees or other bony
prominence areas
Anticipate need for special pressure
mattresses and other devices
Anxiety
› Feelings of apprehension, worry, uneasiness or
dread
Causes:
›
›
›
›
›
›
Medication side effects
Fear of the unknown
Inability to perform tasks at hand
Financial concerns
Family conflicts
Spiritual distress
Listen with empathy
Provide reassurance
Decrease environmental stimuli (turn lights
down, turn off TV, remove from crowded or
loud areas)
Offer to engage in distraction activities
Engage other team members –
multidisciplinary approaches to care
Disorientation to time, place or person
STM loss
Unusual or inappropriate communication
Talking nonsensical
Yelling
Searing
Rudeness
Hallucinations
Gently reorient to person, place and time
› Provide calendar, clock, etc. if appropriate)
Ensure use of hearing aides and eyeglasses
Decrease clutter, keep environment organized
and simple
Pace patient activities, provide rest periods
Use simple, brief instructions
Provide emotional support
›
›
›
›
Reassurance of safety
Calm tone of voice
Avoid arguing
Be patient
Depression: Extreme and ongoing cluster of
feelings that may include: sadness,
hopelessness; helplessness; lack of selfworth; anger;
History of depression
DM; Thyroid disease
Dementia
ETOH
Brain METS
Pain; nausea, diarrhea
Radiation/chemo side effects
Profound loss of control; fear; grief
Spiritual grief; family dysfunction or lack of
support
Provide emotional support to patient – be
present and be a good listener…
Avoid trying to “cheer” patient; maintain
normal level of social conversation
Encourage as much independence and
control as possible; particularly ADL’s
Provide opportunity for talking about and
remembering significant life events
Encourage use of previous helpful coping
mechanisms – prayer, family/friend visits..
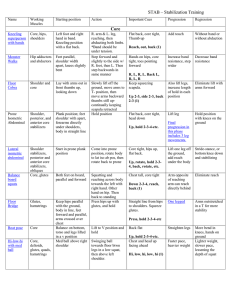
High fowlers
Semi-Fowlers
Supine
Prone
Lateral or side lying position
Right lateral position
Sim’s position
Heels
Pelvis
Spine
Sacrum
Heels
Sacrum
Elbows
Scapulae
Occipital
region (back of head)
Ankle
bone
Knees
Hip bone
Shoulder
Side of the head (parietal region) and
ears
Toes
Knees
Male
genitals
Breasts
Shoulder
Cheek and ears
Ears
Cheek
Shoulder
Hip
Feet
Toes
Providing good skin care
Keep skin clean and dry
Turn and position patients at least every 2
hours (educate your patient,
family/caregivers)
Observe condition of skin and report to nurse
(bathing is an excellent time to do this)
Encourage mobility
Empower patients in the plan of care
Provide
for toileting needs
Encourage and provide nutrition and
fluids (as appropriate)
Use pressure ulcer reducing
cushions, mattresses, beds, booties,
elbow pads, etc.)
Be cognizant of disease process
progression / intervention modalities
Berman, A., Snyder., S., Kozier, B., and Erb,
G. (2010)
Fundamentals of Nursing: Concepts,
Process and Practice. 8th edition.; Pearson
Prentice Hall
Presentation adapted for in-house training
only