Overview of Robert W. Baird & Co.
advertisement
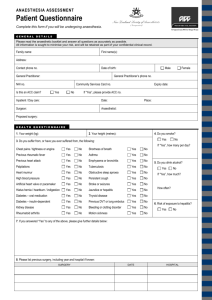
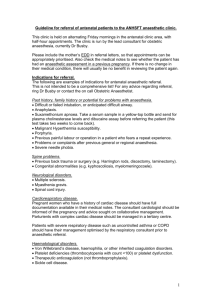
Current Trends in Anaesthetic Practice January 2012 Dr Badrul Amin Siddique DA (London) MRCA (England) at Mymensingh Medical College Hospital Associate Specialist Department of Anaesthetics Royal Orthopaedic Hospital, Birmingham, United Kingdom Agenda Some of the ways in which anaesthesia contributes to the hospital practice ― Preoperative assessment ― Intra operative care and induction of anaesthesia ― Post operative care ― Acute pain management ― Chronic pain management 2 Assessment A preoperative visit from the anaesthetist is appreciated by the patients and is more effective anxiolytic than premedication The aim of preoperative assessment is to ensure that the patient’s health is optimal and that any potential difficulties during anaesthesia are anticipated A thorough medical history should be taken and patient’s general health should be assessed including the drug treatment 3 ASA Scoring System Describes the preoperative condition of a patient and is routinely used in UK ASA physical status rating represents an attempt to estimate anaesthetic and surgical risks according to the severity of the disease process (predicting perioperative morbidity and mortality) 1)Healthy patient (0.1%) 2)Mild systemic disease, no functional limitation (0.2%) 3)Moderate systemic disease, definite functional limitation (1.8%) 4)Severe systemic disease that is a constant threat to life 4 Choice of Air Way According to the need of surgical procedure and position required Mainly used is Laryngeal mask or tracheal intubation Ease of intubation has been graded according to the view obtained on laryngoscopy by Cormack in 1984 ― Grade 1 – whole glottis visible ― Grade 2 – glottis incompletely visible ― Grade 3 – epiglottis but not glottis visible ― Grade 4 – epiglottis not visible 5 Difficult Intubation Some congenital abnormalities and pathological condition may predict a difficult intubation ― Obesity ― Tumour on the neck like goitre (should have x-ray chest and of thoracic inlet) ― Restricted head and neck movement ― Restricted Jaw movement ― Receding mandible ― High upper incisor tooth ― Ankylosing spondiolities of neck ― Short and Bull neck 6 The View Obtained at Layryngoscopy Grade 1 – Visualisation of the vocal cords easily Grade 2 – Visualisation of the posterior portion of the laryngeal aperture Grade 3 – Visualisation of the epiglottis Grade 4 – Visualisation of the soft palate only 7 Indication of Intubation To ensure airway patency and protect the airway from aspiration Intubation trolley must have all types of laryngoscope Intubation trolley must have Gödel airway of different sizes 8 Preparation for Anaesthesia Associated conditions and administration of existing therapy Starvation Fluid status Antibiotic therapy WHO list 9 Choice of Anaesthetic The type of anaesthetic to be used must be decided by the anaesthetist, surgeon and the patient ―Some surgeon may prefer a particular technique where a blood less field is required Patient should be told about the anaesthetic option for the operation such as general versus regional, and versus local infiltration with sedation 1 Methods of Induction Inhalational anaesthetic agents are administered by concentration rather than dose and as the concentration delivered rapidly equilibrates between alveoli, blood and brain, and this allows away of quantifying the anaesthetic effect for each agent To determine the depth and potency of inhalational anaesthetic agent the term MAC (minimal alveolar concentration) used ― MAC is defined as that concentration of anaesthetic agent that will prevent reflex response to a skin incision in 50% of subjects MBC (minimal blood concentration) is another expression of potency ― Another measure of potency is AD95 (anaesthetic dose) or MAC95, which is the alveolar concentration of the agent to produce lack of reflex response to surgery in 95% of subject 11 Methods of Induction (cont’d) Intravenous induction agents are in contrast administered by dose rather concentration ― Commonly used intravenous agents ― Intravenous route of induction is the most common method of induction producing rapid unconsciousness and has a high degree of patient acceptability than inhalational induction Indication for elective inhalational induction ― Airway obstruction or abnormal anatomy ― Difficult or failed intubation ― Patient request 1 Intra-Operative Management for Spontaneous Breathing Monitoring should be commenced before induction of anaesthesia and continued until the patient has recovered from the anaesthetic ― Pulse oximeter, ECG, Capnograph, inspired gas oxygen analyser, fresh gas oxygen analyser, and anaesthetic vapour analyser For Artificial Ventilation – all the plus ― Air pressure gauge ― Ventilation disconnect device ― Ventilation volume ― Peripheral nerve stimulator ― Temperature monitoring and conservation of body heat – bear hugger 1 Maintenance of Anaesthesia The objectives of maintenance of anaesthesia (whatever form it takes) are ― to supply oxygen and remove CO2 from the tissues via the alveoli ― to observe physiological parameters ― to detect, treat or prevent any adverse event ― to pay particular attention to organs at specific risk e.g. kidneys ― to manage fluid balance ― to maintain body temperature ― to produce good operating conditions ― to initiate an analgesic regimen so that the patient does not have severe pain postoperatively 1 Positioning of the Patient Supine Prone Lateral Lithotomy ― Complications 1 Tourniquets Used on the arms and legs to produce a blood less field ―There is a possibility of limb damage with cuff pressure and the duration of inflation ―Recommendations ―Contraindications 1 Conservation of the Body Heat Anaesthetist has a vital role in the maintenance of patient’s body temperature Use of bear hugger is essential for major surgery Hot water electric blanket 1 Conclusion of Maintenance of Anaesthesia For those patient who have received sedation or general anaesthetic and at the end of surgery a satisfactory emergence requires ―return of consciousness with intact laryngeal reflexes and awareness ―return of muscle power with ability to cough and move ―adequate analgesia and hopefully no nausea and vomiting 1 Recovery from Anaesthesia and Postoperative Care Moving the patient from theatre Whether awake or sleep, extubated or not, the patient should not be moved from the operating table until the anaesthetist is satisfied: ― the cardio respiratory status of the patient is satisfactory ― the bed or trolley has an oxygen delivering facilities ― suction equipment is available ― necessary breathing system equipment and sufficient trained staff available 1 Transfer of the Patient to Recovery Ward Staffs On arrival in recovery ward the handover to recovery staff should include the following information: ― Nature of surgery that has taken place including any complications that might affect recovery e.g. excessive blood loos, recent opioid administration ― The site of wound, dressings and drain ― Important aspect of the patients general health e.g. cardiac disease, asthma and others ― The type of anaesthetic given, including details of the regional blocks ― Prescription of postoperative analgesia, antiemetic, and fluids 2 Routine Care Respiratory function ― a respiratory rate of 10 to 20 breaths per minute ― no sign of distress ― normal colour and oxygen saturations reading Cardiovascular function ― the most common cause of hypotension is hypovolaemia ― the most common cause of hypertension is pain Pain management and pain assessment ― Systemic opioids ― Spinal opioids ― Non steroidal – anti-inflammatory drugs 2 Routine Care (cont’d) Post operative nausea and vomiting Post operative fluid therapy Shivering Thrombo – Embolism ― Prophylaxis Physical methods – – – Application of graduated compression or thrombo- embolic deterrent stockings Intermittent compression pumps devices to prevent venous stasis Early ambulation and leg exercises should be encouraged in the post operative period Pharmacological method – Subcutaneous administration of unfractionated and low molecular weight heparin 2 Sequelae of Anaesthesia Complications occurring after surgery results from combinations of factors ― Patient with co morbidity * surgery * anaesthetic Morbidity directly attributable to anaesthetic practice is minor ― Post operative sore throat, and hypoxic brain damage, eye trauma such as corneal abrasions, injury to the teeth, air way trauma, musculoskeletal trauma, backache, neck pain, nerve injuries, facial and supra orbital nerve palsies 2 Conclusion The postoperative anaesthetic care of a patient is often extremely hazardous and may be inadequately unsupervised The careful assessment and prescription of pain relief, oxygen, antiemetics and replacement fluids are the responsibility of the anaesthetist The role of the anaesthetist is increasingly continuing until the patient goes home and is effectively no longer dependent upon specialised hospital care 2