Clinical Anatomy of Nasal Cavity and Olfaction
advertisement
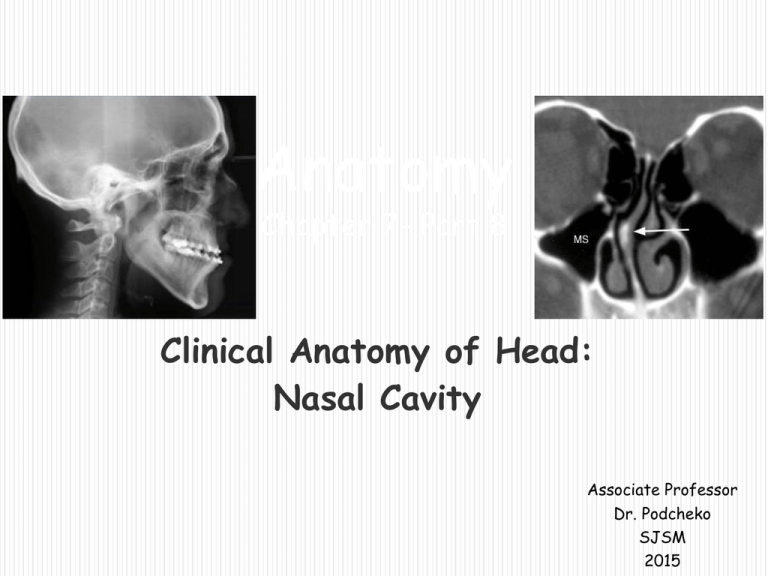
Anatomy Chapter 7- Part 8 Clinical Anatomy of Head: Nasal Cavity Associate Professor Dr. Podcheko SJSM 2015 Intended Learning Outcomes: To know clinical anatomy of : NOSE External Nose Nasal Cavities Vasculature and Innervation of Nose Paranasal Sinuses Clinical correlations related to the nasal cavity anatomy Nose •The nose is the part of the respiratory tract superior to the hard palate and contains the peripheral organ of smell. •It includes the external nose and nasal cavity, which is divided into right and left cavities by the nasal septum. •The functions of the nose are olfaction (smelling), respiration (breathing), filtration of dust, humidification of inspired air, and reception and elimination of secretions from the paranasal sinuses and nasolacrimal ducts. External Nose •The external nose is the visible portion that projects from the face; its skeleton is mainly cartilaginous. •Noses vary considerably in size and shape, mainly because of differences in these cartilages. •The dorsum of the nose extends from the root of the nose to the apex (tip) of the nose. •The inferior surface of the nose is pierced by two piriform (pearshaped) openings, the nares (nostrils, anterior nasal apertures), which are bound laterally by the alae (wings) of the nose. External Nose •The superior bony part of the nose, including its root, is covered by thin skin. •The skin over the cartilaginous part of the nose is covered with thicker skin, which contains many sebaceous glands. •The skin extends into the vestibule of the nose, where it has a variable number of stiff hairs (vibrissae). •Because they are usually moist, these hairs filter dust particles from air entering the nasal cavity. •The junction of the skin and mucous membrane is beyond the hairbearing area. Skeleton of the External Nose •The supporting skeleton of the nose is composed of bone and hyaline cartilage. •The bony part of the nose consists of the nasal bones, frontal processes of the maxillae, the nasal processus of the frontal bone and its nasal spine, and the bony parts of the nasal septum. Skeleton of the External Nose, contd. •The cartilaginous part of the nose consists of five main cartilages: two lateral cartilages, two alar cartilages, and one septal cartilage. •The U-shaped alar cartilages are free and movable; they dilate or constrict the nares when the muscles acting on the nose contract. Nasal Septum •The nasal septum divides the chamber of the nose into two nasal cavities and has a bony part and a soft mobile cartilaginous part. •The main components of the nasal septum are the perpendicular plate of the ethmoid, the vomer, and the septal cartilage. •The thin perpendicular plate of the ethmoid bone, forming the superior part of the nasal septum, descends from the cribriform plate and is continued superior to this plate as the crista galli. •The vomer, a thin flat bone, forms the posteroinferior part of the nasal septum, with some contribution from the nasal crests of the maxillary and palatine bones. •The septal cartilage has a tongueand-groove articulation with the edges of the bony septum. Clinical Correlates: Nasal Fractures •Because of the prominence of the nose, fractures of the nasal bones are common facial fractures in automobile accidents and sports (unless face guards are worn). •Fractures usually result in deformation of the nose, particularly when a lateral force is applied by someone's elbow, for example. •Epistaxis (nosebleed) usually occurs. •In severe fractures, disruption of the bones and cartilages results in displacement of the nose. •When the injury results from a direct blow, the cribriform plate of the ethmoid bone may also fracture. Deviation of the Nasal Septum •The nasal septum is usually deviated to one side or the other. •This could be the result of a birth injury, but more often the deviation results during adolescence and adulthood from trauma (e.g., during a fist fight). •Sometimes the deviation is so severe that the nasal septum is in contact with the lateral wall of the nasal cavity and often obstructs breathing or exacerbates snoring. •The deviation can be corrected surgically. Nasal Cavity •The term nasal cavity, divided into right and left halves by the nasal septum, refers to either the entire cavity or one of its halves, depending on the context. •The nasal cavity is entered anteriorly through the nostrils. •It opens posteriorly into the nasopharynx through the choanae. •Mucosa lines the nasal cavity covered with ciliated columnar epithelium containing goblet cells and serous glands. The serous glands produce a fluid containing lysozymes which are bacteriocidal •Nasal vestibule is lined with skin. Nasal Cavity, contd. •The nasal mucosa is firmly bound to the periosteum and perichondrium of the supporting bones and cartilages of the nose. •The mucosa is continuous with the lining of all the chambers with which the nasal cavities communicate: the nasopharynx posteriorly, the paranasal sinuses superiorly and laterally, and the lacrimal sac and conjunctiva superiorly. Nasal Cavity, contd. •The inferior two thirds of the nasal mucosa is the respiratory area and the superior one third is the olfactory area. •Air passing over the respiratory area is warmed and moistened before it passes through the rest of the upper respiratory tract to the lungs. •The olfactory area contains the peripheral organ of smell; sniffing draws air to the area Boundaries of the Nasal Cavity •The nasal cavity has a roof, floor, and medial and lateral walls. •The roof of the nasal cavity is curved and narrow, except at its posterior end; it is divided into three parts (frontonasal, ethmoidal, and sphenoidal) named from the bones forming each part. 1 2 3 Boundaries of the Nasal Cavity •The floor of the nasal cavity is wider than the roof and is formed by the palatine processes of the maxilla and the horizontal plates of the palatine bone. •The medial wall of the nasal cavity is formed by the nasal septum. •The lateral walls of the nasal cavity are irregular owing to three bony plates, the nasal conchae, which project inferiorly, somewhat like louvers (window blinds) Features of the Nasal Cavity •The nasal conchae (superior, middle, and inferior) curve inferomedially, hanging like short curtains. •The conchae (shells) or turbinates of many mammals (especially running mammals and those existing in extreme environments) are highly convoluted, scroll-like structures that offer a vast surface area for heat exchange. Features of the Nasal Cavity • Each nasal conch with surrounding structures forms a recess and/or meatus which underlies each of the conchae •The nasal cavity is divided into five passages: a posterosuperiorly placed sphenoethmoidal recess, three laterally located nasal meatus (superior, middle, and inferior meatus), and a medially placed common nasal meatus into which the four lateral passages open. common nasal meatus Features of the Nasal Cavity •The inferior concha is the longest and broadest and is formed by an independent bone (of the same name, inferior concha) covered by a mucous membrane that contains large vascular spaces that can enlarge to control the caliber of the nasal cavity. •When infected or irritated, the mucosa may swell rapidly, blocking the nasal passage(s) on that side. Features of the Nasal Cavity The sphenoethmoidal recess, lying superoposterior to the superior concha, receives the opening of the sphenoidal sinus, an air-filled cavity in the body of the sphenoid. The superior nasal meatus is a narrow passage between the superior and the middle nasal conchae into which the posterior ethmoidal sinuses open by one or more orifices. Features of the Nasal Cavity •The middle nasal meatus is longer and deeper than the superior one. •The anterosuperior part of this passage leads into a funnel-shaped opening, the ethmoidal infundibulum, through which it communicates with the frontal sinus. •The passage that leads inferiorly from each frontal sinus to the infundibulum is the frontonasal duct. Features of the Nasal Cavity •The semilunar hiatus (hiatus semilunaris) is a semicircular groove into which the frontal sinus opens. •The ethmoidal bulla (bubble), a rounded elevation located superior to the hiatus, is visible when the middle concha is removed. •The bulla is formed by middle ethmoidal cells that form the ethmoidal sinuses. Features of the Nasal Cavity •The inferior nasal meatus is a horizontal passage inferolateral to the inferior nasal concha. •The nasolacrimal duct, which drains tears from the lacrimal sac, opens into the anterior part of this meatus. Vasculature and Innervation of the Nose The arterial supply of the medial and lateral walls of the nasal cavity is from five sources: 1. Anterior ethmoidal artery (from the ophthalmic artery). 2. Posterior ethmoidal artery (from the ophthalmic artery). 3. Sphenopalatine artery (from the maxillary artery). 4. Greater palatine artery (from the maxillary artery). 5. Septal branch of the superior labial artery (from the facial artery). Vasculature and Innervation of the Nose •The first three arteries (anterior ethmoidal artery, posterior ethmoidal artery and sphenopalatine artery) divide into lateral and medial (septal) branches. •The greater palatine artery reaches the septum via the incisive canal through the anterior hard palate. •The anterior part of the nasal septum is the site (Kiesselbach area) of an anastomotic arterial plexus involving all five arteries supplying the septum. •The external nose also receives blood from first and fifth arteries listed above plus nasal branches of the infraorbital artery and the lateral nasal branches of the facial artery. Vasculature and Innervation of the Nose •A rich submucosal venous plexus deep to the nasal mucosa drains into the sphenopalatine, facial, and ophthalmic veins. •This venous plexus is an important part of the body's thermoregulatory system, exchanging heat and warming air before it enters the lungs. •Venous blood from the external nose drains mostly into the facial vein via the angular and lateral nasal veins [lies within the ‘danger area’ of the face because of communications with the cavernous (dural venous) sinus]. Innervation of the Nose •Nerve supply - the nasal mucosa can be divided into posteroinferior and anterosuperior portions by an oblique line passing approximately through the apex of the nose and the sphenoethmoidal recess. •The nerve supply of the posteroinferior portion of the nasal mucosa is chiefly from the maxillary nerve, by way of the nasopalatine nerve to the nasal septum, and posterior superior lateral nasal and inferior lateral nasal branches of the greater palatine nerve to the lateral wall. Innervation of the Nose •The nerve supply of the anterosuperior portion is from the ophthalmic nerve (CN V1) by way of the anterior and posterior ethmoidal nerves, branches of the nasociliary nerve. •Most of the external nose (dorsum and apex) is also supplied by CN V1 (via the infratrochlear nerve and the external nasal branch of the anterior ethmoidal nerve), but the alae are supplied by the nasal branches of the infraorbital nerve (CN V2). Innervation of the Nose •The olfactory nerves, concerned with smell, arise from cells in the olfactory epithelium in the superior part of the lateral and septal walls of the nasal cavity. •The central processes of these cells (forming the olfactory nerve) pass through the cribriform plate and end in the olfactory bulb, the rostral expansion of the olfactory tract. Rhinitis •The nasal mucosa becomes swollen and inflamed (rhinitis) during severe upper respiratory infections and allergic reactions (e.g., hayfever). •Swelling of the mucosa occurs readily because of its vascularity. •Infections of the nasal cavities may spread to the: •Anterior cranial fossa through the cribriform plate. •Nasopharynx and retropharyngeal soft tissues. •Paranasal sinuses. •Middle ear through the pharyngotympanic tube (auditory tube), which connects the tympanic cavity and nasopharynx. •Lacrimal apparatus and conjunctiva. Epistaxis •Epistaxis (nosebleed) is relatively common because of the rich blood supply to the nasal mucosa. •In most cases, the cause is trauma and the bleeding is from an area in the anterior third of the nose (Kiesselbach area). •Epistaxis is also associated with infections and hypertension. •Spurting of blood from the nose results from rupture of arteries. •Mild epistaxis may also result from nose picking, which tears veins in the vestibule of the nose. Question: A young child is brought to your office by his mother, who is concerned about his frequent nosebleeds. Nosebleeds often arise from the anteroinferior part of the nasal septum, which is richly vascularized and exposed to the drying effect of air. Which of the following arteries directly supplies that part of the septum? External carotid artery Anterior ethmoidal artery Lesser palatine artery Infraorbital artery Paranasal Sinuses •The paranasal sinuses are air-filled extensions of the respiratory part of the nasal cavity into the following cranial bones: frontal, ethmoid, sphenoid, and maxilla. •They are named according to the bones in which they are located. •The sinuses continue to invade the surrounding bone, and marked extensions are common in the crania of older individuals. Sinusitis •Because the paranasal sinuses are continuous with the nasal cavities through apertures that open into them, infection may spread from the nasal cavities, producing inflammation and swelling of the mucosa of the sinuses (sinusitis) and local pain. •Sometimes several sinuses are inflamed (pansinusitis), and the swelling of the mucosa may block one or more openings of the sinuses into the nasal cavities. Frontal Sinuses •The frontal sinuses are between the outer and the inner tables of the frontal bone, posterior to the superciliary arches and the root of the nose. •Frontal sinuses are usually detectable in children by 7 years of age. •Each sinus drains through a frontonasal duct into the ethmoidal infundibulum, which opens into the semilunar hiatus of the middle nasal meatus. •The frontal sinuses are innervated by branches of the supraorbital nerves (CN V1). Variation of the Frontal Sinuses •The right and left frontal sinuses are rarely of equal size, and the septum between them is not usually situated entirely in the median plane. •The frontal sinuses vary in size from approximately 5 mm to large spaces extending laterally into the greater wings of the sphenoid. •Often a frontal sinus has two parts: a vertical part in the squamous part of the frontal bone and a horizontal part in the orbital part of the frontal bone. •One or both parts may be large or small. •When the supraorbital part is large, its roof forms the floor of the anterior cranial fossa and its floor forms the roof of the orbit. Ethmoidal Cells •The ethmoidal cells (sinuses) are small invaginations of the mucous membrane of the middle and superior nasal meatus into the ethmoid bone between the nasal cavity and the orbit. •The ethmoidal cells usually are not visible in plain radiographs before 2 years of age but are recognizable in CT scans. •The anterior ethmoidal cells drain directly or indirectly into the middle nasal meatus through the ethmoidal infundibulum. Ethmoidal Cells •The middle ethmoidal cells open directly into the middle meatus and are sometimes called ‘bullar cells’ because they form the ethmoidal bulla, a swelling on the superior border of the semilunar hiatus. •The posterior ethmoidal cells open directly into the superior meatus. •The ethmoidal cells are supplied by the anterior and posterior ethmoidal branches of the nasociliary nerves (CN V1). Infection of the Ethmoidal Cells •If nasal drainage is blocked, infections of the ethmoidal cells may break through the fragile medial wall of the orbit. •Severe infections from this source may cause blindness because some posterior ethmoidal cells lie close to the optic canal, which gives passage to the optic nerve and ophthalmic artery. •Spread of infection from these cells could also affect the dural nerve sheath of the optic nerve, causing optic neuritis. Sphenoidal Sinuses •The sphenoidal sinuses are located in the body of the sphenoid and may extend into the wings of this bone. •They are unevenly divided and separated by a bony septum. •Because of this extensive pneumatization (formation of air cells or sinuses), the body of the sphenoid is fragile. Sphenoidal Sinuses •Only thin plates of bone separate the sinuses from several important structures: the optic nerves and optic chiasm, the pituitary gland, the internal carotid arteries, and the cavernous sinuses. •The sphenoidal sinuses are derived from a posterior ethmoidal cell that begins to invade the sphenoid at approximately 2 years of age. •In some people, several posterior ethmoidal cells invade the sphenoid, giving rise to multiple sphenoidal sinuses that open separately into the sphenoethmoidal recess. •The posterior ethmoidal arteries and posterior ethmoidal nerve supply the sphenoidal sinuses. Maxillary Sinuses •The maxillary sinuses are the largest of the paranasal sinuses. •They occupy the bodies of the maxillae and communicate with the middle nasal meatus. Maxillary Sinuses •The apex of the maxillary sinus extends toward and often into the zygomatic bone. •The base of the maxillary sinus forms the inferior part of the lateral wall of the nasal cavity. •The roof of the maxillary sinus is formed by the floor of the orbit. •The floor of the maxillary sinus is formed by the alveolar part of the maxilla. •The roots of the maxillary teeth, particularly the first two molars, often produce conical elevations in the floor of the sinus. Maxillary Sinuses •Each maxillary sinus drains by one or more openings, the maxillary ostium (ostia), into the middle nasal meatus of the nasal cavity by way of the semilunar hiatus. •The arterial supply of the maxillary sinus is mainly from superior alveolar branches of the maxillary artery; however, branches of the descending and greater palatine arteries supply the floor of the sinus. •Innervation of the maxillary sinus is from the anterior, middle, and posterior superior alveolar nerves, which are branches of the maxillary nerve. Infection of the Maxillary Sinuses •The maxillary sinuses are the most commonly infected, probably because their ostia are commonly small and are located high on their superomedial walls. •When the mucous membrane of the sinus is congested, the maxillary ostia are often obstructed. •Because of the high location of the ostia, when the head is erect it is impossible for the sinuses to drain until they are full. •When lying on one's side only the upper sinus (e.g., the right sinus if lying on the left side) drains. •A cold or allergy involving both sinuses can result in nights of rolling from side-to-side in an attempt to keep the sinuses drained. •A maxillary sinus can be cannulated and drained by passing a cannula from the nostrils through the maxillary ostium into the sinus. Relationship of the Teeth to the Maxillary Sinus •The close proximity of the three maxillary molar teeth to the floor of the maxillary sinus poses potentially serious problems •During removal of a molar tooth, a fracture of a root may occur. •If proper retrieval methods are not used, a piece of the root may be driven superiorly into the maxillary sinus. •A communication may be created between the oral cavity and the maxillary sinus as a result, and an infection may occur. •Because the superior alveolar nerves (branches of the maxillary nerve) supply both the maxillary teeth and the mucous membrane of the maxillary sinuses, inflammation of the mucosa of the sinus is frequently accompanied by a sensation of toothache in the molar teeth. A patient presents to your office with nasal congestion, postnasal drip, and extremely uncomfortable pain and pressure in her "cheekbone" (the region between her eye and upper teeth). You determine that she has a severe sinus infection. Which of her paranasal sinuses is most likely involved with this infection? A. Ethmoidal B. Maxillary C. Sphenoidal D. Frontal Teaching Point: Nasal congestion and postnasal drip are signs of an infection. The pain in her maxillary area pinpoints the location of the infection to the maxillary sinus. Transillumination of the Sinuses •Transillumination of the maxillary sinuses is performed in a darkened room. •A bright light is placed in the patient's mouth on one side of the hard palate. •The light passes through the maxillary sinus and appears as a crescent-shaped, dull glow inferior to the orbit. •If a sinus contains excess fluid, a mass, or a thickened mucosa, the glow is decreased. Transillumination of the Sinuses •The frontal sinuses can also be transilluminated by directing the light superiorly under the medial aspect of the eyebrow, normally producing a glow superior to the orbit. •Because of the great variation in the development of the sinuses, the pattern and extent of sinus illumination differs from person to person. •The ethmoidal and sphenoidal sinuses cannot be examined by transillumination. END