Aspirin for the prevention of recurrent venous Thromboembolism (VTE)
advertisement
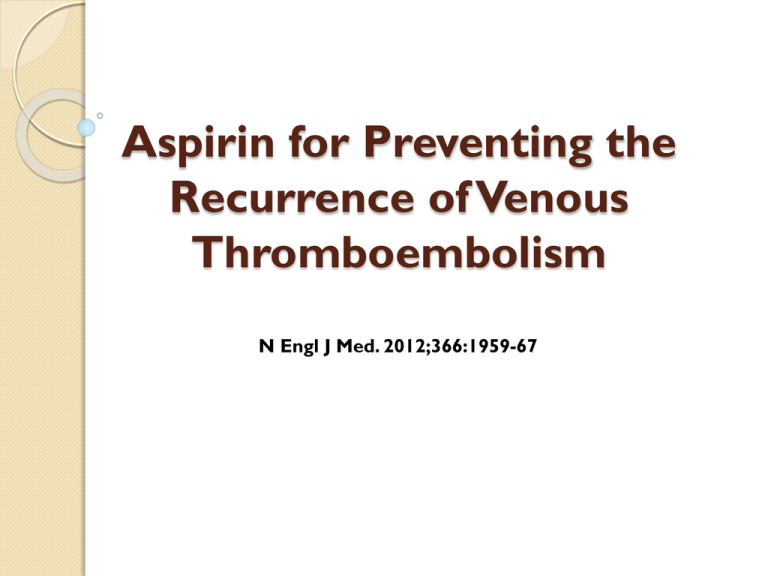
Aspirin for Preventing the
Recurrence of Venous
Thromboembolism
N Engl J Med. 2012;366:1959-67
VTE Prevalence
Incidence of DVT: 48 per 100,000
Incidence of PE: 23 per 100,000
Case-fatality rate
◦ Inpatient: 12%
◦ 1-year: 19%; 3-year: 30%
Extrapolated data: 170K new cases/year of VTE
in US diagnosed as inpatients, 99K recurrent
hospitalizations
VTE Prevalence
Prevalence of asymptomatic DVT in
patients not receiving prophylaxis
(Geerts, Chest 2008)
◦ Internal: 10-20%
◦ Stroke 20-50%, Critical care 10-80%
◦ General Surgery: 15-40%
VTE Outcomes
DVT outcomes (Prandoni, Haematologica 1997)
◦
◦
◦
◦
Mortality usually related to underlying illness
Morbidity
17% 2-year risk of recurrence (initial rx 3 months)
25% 2-year risk of post-thrombotic syndrome
PE outcomes (Goldhaber, Lancet 1999)
◦ Mortality: 17% at 3-months
Worse in elderly patients (Kniffin, Arch Intern Med 1994)
◦ 21% in-hospital & 39% 1-year mortality for PE
VTE Costs
Inpatient complications (Zhan, JAMA 2003)
◦ 3rd most common hospital complication,
behind obstetrical trauma & decubitus ulcers
◦ Excess LOS: 5.4 days
◦ Excess charges: $21,709
◦ Excess mortality: 6.5%
Virchow’s Triad
Stasis
Trauma
Hypercoaguability
Virchow RLK (1856). "Thrombose und Embolie. Gefässentzündung und septische Infektion". Gesammelte
Abhandlungen zur wissenschaftlichen Medicin. Frankfurt am Main:Von Meidinger & Sohn. pp. 219–732.Translation in
Matzdorff AC, Bell WR (1998). Thrombosis and embolie (1846-1856). Canton, Massachusetts: Science History
Publications.
Risk Factors for VTE
Age
Prior VTE
Surgery, trauma
Immobility
Pregnancy/postpartum
Medical illness
◦
◦
◦
◦
Cancer & cancer rx
Inflammatory Bowel Dz
Nephrotic Syndrome
Obesity
Meds
◦
◦
◦
◦
Hormone replacement
Tamoxifen, raloxifene
Cancer drugs
Erythropoetin
Thrombophilia
◦ Inherited
◦ Acquired
Risk Factors for VTE
Age
Prior VTE
Surgery, trauma
Immobility
Pregnancy/postpartum
Medical illness
◦
◦
◦
◦
Cancer & cancer rx
Inflammatory Bowel Dz
Nephrotic Syndrome
Obesity
Meds
◦
◦
◦
◦
Hormone replacement
Tamoxifen, raloxifene
Cancer drugs
Erythropoetin
Thrombophilia
◦ Inherited
◦ Acquired
Almost all inpatients have 1 RF
40% of inpatients have ≥3 RF
Risk Stratification
Risk Categories
◦ Low Risk (<10%)
◦ Moderate Risk (10-40%)
◦ High Risk (40-80%)
Risk
Type
Rx
Low
Minor surgery &
medical, mobile
Early ambulation
Moderate
Most general
surgery & medical
patients
Medical +/mechanical
High
Ortho & major
trauma
Medical +/mechanical
Bleeding Risk
Active bleeding
Severe trauma to head
or SC with hemorrhage
within 4 weeks
ICH within 1 year
Craniotomy within 2
weeks
Intraocular surgery
within 2 weeks
GI/GU hemorrhage
within last month
Post-op bleeding
concerns
Thrombocytopenia
(<50K)
Coagulopathy
End stage liver disease
Active intracranial
lesions/neoplasm
Hypertensive emergency
Other Considerations
Heparin-induced thrombocytopenia (HIT)
◦ If hx, no LDUH or LMWH at any doses
◦ Fondaparinux OK
Epidural analgesia with indwelling catheter
Renal dysfunction
◦ Renally dose LMWH, consider avoidance in
pts with severely reduced CrCl
◦ Avoid fondaparinux in pts with CrCl <30
VTE Prophylaxis
Prophylaxis Choices
Early & frequent ambulation
Mechanical
◦ Graduated compression stockings (GCS)
◦ Intermittent pneumatic compression (IPC)
Medical
◦
◦
◦
◦
◦
Aspirin
Low-dose Unfractionated Heparin (LDUH)
Low Molecular Weight Heparin (LMWH)
Fondaparinux (Arixtra©)
Warfarin (Coumadin©)
Mechanical Prophylaxis
Multiple studies have shown benefit to reduce risk of
DVT (no studies large enough to show reduction in PE
or mortality)
But, less evidence to support use and less effective than
medical prophylaxis
Must be properly fitted, applied, and worn almost
continuously
Reserve for use in patients with high bleeding risk (or as
adjunctive therapy to medical prophylaxis in certain high
risk patients) & reassess bleeding risk frequently
Minimal contraindications: severe PVD; amputees can
use upper extremity IPCs
Low Dose Unfractionated Heparin
5000 units SQ BID-TID
◦ TID dosing is more physiologic, but little head-tohead evidence it is better than BID
Reduced incidence of DVT, PE, fatal PE
Incidence of major bleeding is low: 0.3 to 2
cases/1000 patient days
HIT is possible (3% risk of thrombocytopenia),
monitor platelets regularly
Low Molecular Weight Heparin
Multiple choices: enoxaparin, dalteparin,
tinzaparin, nadroparin, rivaparin, certoparin
Enoxaparin: 40 mg SQ QD (or 30 mg SQ BID)
Renal dose adjustment: 30 mg QD (or avoid if
CrCl <30)
HIT risk lower than LDUH (0.4%), but still
monitor platelets
Warfarin
Variable dosing, usually start at 5-10 mg daily; adjust per INR
Takes at least 48 hrs to have measurable effect on
coagulation, and may take 5-7 days to be clinically effective
Requires close monitoring
No standard renal adjustment (although higher risk of
bleeding)
Usually reserved for longer-term prophylaxis situations
(ortho procedures)
Effective in patients already
on for another indication (i.e.
nd
don’t need to add a 2 agent)
Long term anticoagulation (warfarin INR 2-3) is
effective however…
• causes major (fatal) bleeding
• inconvenient for patients (warfarin)
Aspirin so far…
Main evidence for use
◦ Antiplatelet Trialists’ Collaboration (BMJ 1994): Metanalysis of
>50 trials, many quite old & of questionable validity; Significant
reduction in DVT rates with ASA
◦ PEP trial (Lancet, 2000): Significant reductions in VTE with 160 mg
ASA QD in post-op ortho patients (NNT ~250 to prevent fatal
PE, ~111 for any VTE event)
2008 ACCP guidelines recommend against ASA as
primary form of VTE prophylaxis
Does aspirin reduce recurrence of venous
thromboembolism (VTE) after a course
of oral vitamin K antagonist therapy in
adults with a first-ever, unprovoked VTE?
Methods
Double Blinded Randomized placebocontrolled trial (Aspirin for the
Prevention of Recurrent Venous
Thromboembolism [Warfarin and Aspirin
{WARFASA}] study)
Patients
403 patients >18 years of age (mean age 62 y, 64%
men) who had a first-ever, objectively confirmed,
symptomatic, unprovoked (without known risk
factors), proximal deep venous thrombosis (DVT),
pulmonary embolism (PE), or both.
Received oral vitamin K antagonists for 6 to 18
months (target interna-tional normalized ratio of
2.0 to 3.0), and were randomized within 2 weeks
of anticoagulant withdrawal
Intervention : Aspirin, 100 mg once daily (n=
205), or placebo (n= 198) for 2 years.
Follow-up period : Median 25 months.
Setting: 25 centers in Austria and Italy
Outcomes
Primary efficacy outcome was symptomatic,
objectively verified, recurrence of VTE
(composite of DVT or PE).
Primary safety outcome was major bleeding
(fatal, occurring in a critical site, ≥2.0-g/dL
decrease in hemoglobin, or transfusion of ≥2
units of whole blood or red cells).
Secondary outcomes included DVT; PE;
clinically relevant, non major bleeding; and
mortality
Results
Results
Aspirin reduced recurrent VTE and DVT more than
placebo
Groups did not differ for PE, bleeding, or mortality
Conclusion
After discontinuation of anticoagulant therapy
for a first-ever, unprovoked venous
thromboembolism, aspirin reduced recurrence.
Aspirin is an effective option for patients unable
or who do not wish to continue anticoagulation
beyond their initial therapy
◦
◦
◦
◦
◦
Simple therapy
Widely available
Low cost
Well tolerated with low risks bleeding
Benefits not solely restricted to prevention of
recurrent VTE
Comments
Patients with an unprovoked VTE are treated
with oral anticoagulation for ≥3 months. The risk
for recurrence of VTE is approximately 25% in 5
years.
Assessment of risk for recurrent VTE - The
DASH Score - D-dimer, Age, Sex, Hormonal
therapy –
◦ An abnormal D-dimer measurement after
anticoagulation is stopped
◦ <50 years of age
◦ Male sex
◦ VTE not associated with hormone therapy in women
Comments
This study needs to be assessed in the context of
the similar, but larger, ongoing ASPIRE study.
If the results are confirmed, there would be
compelling data to support the use of aspirin,
with its low cost and toxicity, to treat patients
with low, and possibly intermediate, risk for VTE
after ≥3 months of anticoagulation treatment.
Patients at high risk for recurrent VTE not at high
risk for bleeding would benefit more from
extended anticoagulation therapy given in the
article
The Next level… ASPIRE Study
822 randomized
6 not qualifying
DVT
411 assigned
placebo
411 assigned
aspirin
411 received
placebo
411 received
aspirin
2 revoked consent
10 revoked consent
4 lost to follow-up
6 not qualifying DVT
2 lost to follow-up
411 included
in analysis
411 included
in analysis
First patient enrolled May 2003,
Last patient enrolled August 2011,
Follow-up completed March 2012
Primary Outcome - Recurrent VTE
Cumulative risk
0.3
HR = 0.74 (95% CI: 0.52-1.05),
p=0.09
0.2
Placebo
Aspirin
0.1
0
0
No. at risk
1
2
3
4
Years since randomization
Placebo
411
341
282
205
135
Aspirin
411
369
299
217
151
Major Vascular and Net Clinical Benefit
0.3
0.3
Cumulative risk
HR: 0.66 (0.48–0.92)
p=0.01
HR: 0.67 (0.49–0.91)
p=0.01
0.2
Placebo
0.2
Placebo
0.1
0
0
Aspirin
Aspirin
1
2
3
0.1
4
0
0
1
Years from randomisation
2
3
4
Meta-analysis ASPIRE & WARFASA
Outcome & study
Placebo Aspirin
events/n events/n
Hazard Ratio (95% CI)
Hazard Ratio P
ASPIRE 73/411 57/411
0.74
0.09
WARFASA43/197 28/205
0.58
0.02
Pooled 116/608 85/616
0.68
0.007
ASPIRE 88/411 62/411
0.66
0.01
WARFASA48/197 36/205
0.67
0.06
Pooled 136/608 98/616
0.66
0.002
Clinically ASPIRE 8/411 14/411
relevant WARFASA 4/197 4/205
bleeds
Pooled 12/608 18/616
1.72
0.22
0.98
0.97
1.47
0.31
VTE
Major
vascular
events
0.2
0.5
Favors Aspirin
1
2
Favors Placebo
5
Thank You !!!