Reproductive System
advertisement
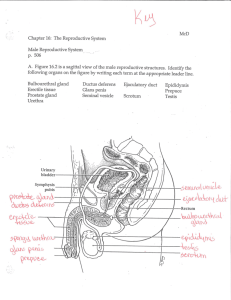
Reproductive System Objectives: 1. 12.0 Identify structures and functions of the reproductive system 2. 12.1 Differentiating between male and female reproductive systems 3. 12.3 Identifying disorders of the reproductive system Examples: endometriosis, sexually transmitted diseases, prostate cancer Preassessment Quiz 1. 2. 3. 4. 5. 6. 7. 8. 9. What is a male sex cell called? What is the male primary sex organ? What do the primary sex organs do? Name 2 internal male accessory organs. Name 2 external male accessory organs. What is a female sex cell called? What is the female primary sex organ? Name 2 internal female accessory organs. Name 2 external female accessory organs. Organs of the Male Reproductive System • Label and color Figure 19.1 1. Testes • Enclosed in a tough, white, fibrous capsule (tunica albuginea) within the scrotum (2.) • Connective tissue thickens along inferior border of capsule and projects into testis, dividing it into 250 lobules • Each lobule contains 1-4 highly convoluted seminiferous tubules. Testes, continued….. • Seminiferous tubules join in a complex network called the rete testis. • Ducts branching off the rete testis join a single, convoluted tube called the epididymis (3.) • Once the epididymis straightens, it becomes the vas deferens (4.) Structure of the Testes, continued….. • What does spermatogenic mean? • Inside the seminiferous tubules: – Spermatogenic cells (specialized epithelial cells) line the walls. – They form sperm cells that collect in the lumen of the tubule. • Between the tubules are interstitial cells (“cells of Leydig”), which produce male sex hormones. Testicular Cancer • Arises from the epithelial cells of the seminiferous tubules. (What are the names of these cells?) • Signs: – Painless swelling of the testis – Scrotal mass attached to the testis • Treatments: – Surgical removal of testis – Radiation and/or chemotherapy Formation of Sperm Cells • Where are they formed??? • Males produce sperm cells continually throughout their reproductive lives. • They collect in the lumen and pass to the epididymis, where they mature and accumulate. Formation of Sperm Cells, continued….. • 3 main parts: 1.Head a. Mainly a nucleus containing 23 chromosomes b. Acrosome – a projection at the end of the head that contains enzymes to assist in penetrating an egg 2.Midpiece - contains many mitochondria 3.Tail - flagella; function???? Spermatogenesis • Mitosis vs. meisosis Spermatogenesis, continued….. Male Internal Accessory Organs 1. Epididymis 2. Vas deferens 3. Seminal vesicle 4. Prostate gland 5. Bulbourethral glands 6. Semen (*) 3. Epididymis • Convoluted tube that is connected to ducts within the testis, emerges from the top of the testis, descends along the posterior surface of the testis, and ascends to become the vas deferens. • Immature, nonmotile sperm mature as they are moved through the epididymis. 4. Vas deferens • Travels from epididymis to just behind the bladder • Unites with the duct of a seminal vesicle (5) to form an ejaculatory duct (6) • Ejaculatory duct passes through the prostate gland (7) and empties into the urethra (8) 5. Seminal vesicle • Convoluted sac-like structure attached to the vas deferens near the base of the urinary bladder • Secretes: – a slightly alkaline fluid to regulate pH of tubular contents – fructose to provide energy to sperm cells – prostaglandins to stimulate muscular contractions in female reproductive organs to help move sperm cells 7. Prostate Gland • Chestnut-shaped structure that surrounds proximal portion of urethra • Ducts open into urethra • Secretes thin, milky, alkaline fluid – Neutralizes acidic fluid containing sperm cells – Neutralizes acidic vaginal secretions – Enhances motility of sperm cells 10. Bulbourethral Glands • AKA, Cowper’s glands • Located inferiorly to the prostate gland, within muscle fibers of external urethral sphincter • Secretes mucuslike fluid to lubricate the end of the penis for sexual intercourse • (As always, females do most of the work of producing lubricating fluid. :) Semen • The fluid the male urethra releases during ejaculation • Consists of: – Sperm cells – Secretions of the seminal vesicles, prostate gland, and bulbourethral glands • About 120 million sperm cells/mL semen • 2-5 mL semen released at a time Enlarged Prostate Gland • Where is the prostate gland located??? • So, what would happen if the prostate gland became enlarged? • Testing for prostate cancer: – Rectal exam – PSA (prostate-specific antigen) blood test to check for a cell surface protein found on prostate cells – Ultrasound Treatment Options for Enlarged Prostate Gland • Surgical removal of prostate • Radiation • Microwave energy delivered through a probe inserted into the urethra or rectum • Freeze tumor with liquid nitrogen delivered by a probe through the skin • Others Male External Accessory Organs 1. Scrotum 2. Penis 2. Scrotum • 1.Pouch of skin that houses the testes • 2. Medial septum divides it into 2 chambers • 3. Protects and aids in temperature regulation of the testes 11. Penis • Conveys urine and semen through the urethra to the outside • The body (shaft) has 3 columns of erectile tissue: 1. A pair of dorsally located corpora cavernosa (12) 2. A single, ventral corpus spongiosum (13) 11. Penis, continued….. • Corpus spongiosum: – Urethra passes through it – Enlarges at distal end to form the glans penis (14) • Glans penis – Covers the ends of the corpora cavernosa – Bears urethral opening (orifice) – Contains sensory receptors • Prepuce (15) – fold of skin that covers the glans penis; removed in circumcision Erection, Orgasm, and Ejaculation • Sexual stimulation leads to parasympathetic nerve impulses from the spinal cord to release NO, a vasodilator. • Arteries leading to the penis dilate. • Pressure from arterial blood filling the vascular spaces of erectile tissue compress the penis veins. • Venous blood cannot flow out of the penis, erectile tissue fills, and an erection is produced. Erection, Orgasm, and Ejaculation, continued….. • Emission and ejaculation accompany male orgasm. • Emission: the movement of sperm cells from the testes and secretions from the prostate gland and seminal vesicles into the urethra. • Ejaculation: the process of forcing semen through the urethra to the outside Erection, Orgasm, and Ejaculation, continued….. • Emission and ejaculation events occur so that: 1.Fluid from bulbourethral glands is expelled first 2.Fluid from the prostate gland is released next 3.Then sperm cells 4.Lastly, fluid from the seminal vesicles Erection, Orgasm, and Ejaculation, continued….. • Following ejaculation: • Arteries that supply erectile tissue contract, • Veins of the penis “drain” the spaces of the erectile tissue, • Penis returns to flaccid state Hormonal Control of Male Reproductive Functions • Hormones are secreted by: – Hypothalamus – Anterior pituitary gland – Testes • Functions: – Development of sperm cells – Development of secondary sex characteristics Hypothalamic and Pituitary Hormones • Hypothalamus secretes gonadotropin-releasing hormone (GnRH) to anterior pituitary gland • In response, anterior pituitary gland secretes gonadotropins: 1. Luteinizing hormone (LH) 2. Follicle-stimulating hormone (FSH), aka interstitial cell-stimulating hormone (ICSH) Hypothalamic and Pituitary Hormones, continued….. • FSH (ICSH) promotes development of ___________. • Testicular interstitial cells secrete male sex hormones. • LH stimulates supporting cells of seminiferous tubules to respond to testosterone. Hypothalamic and Pituitary Hormones, continued….. • FSH + testosterone + supporting cells stimulate spermatogenic cells to give rise to ______________. • Supporting cells secrete inhibin, a hormone which inhibits the anterior pituitary gland, preventing secretion of FSH. Male Sex Hormones • Called “Androgens” (???) • Where are they produced? • Most in testicular interstitial cells, but small amounts in adrenal cortex • What is the main male sex hormone? • Testosterone production begins before birth, continues a few weeks after, and then ceases until puberty. Actions of Testosterone • Stimulates enlargement of testes and male accessory organs • Stimulates development of male secondary sex characteristics: 1. Increased growth of body hair 2. Enlargement of the larynx and thickening of the vocal cords 3. Thickening of the skin 4. Muscle growth, widening of shoulders, narrowing of waist 5. Thickening and strengthening of bones Actions of Testosterone, continued….. • Increases rate of cellular metabolism • Increases rate of RBC production Regulation of Male Sex Hormones • More testosterone = more developed secondary sex characteristics • Increased levels of testosterone inhibit the hypothalamus. • What effects would inhibition of the hypothalamus have? Organs of the Female Reproductive System • Label Figure 19.7 1. Ovaries • Ovarian tissues are subdivided: – Inner medulla – Outer ______ • Ovarian cortex appears granular due to tiny masses of cells called ovarian follicles (19). Ovaries, continued….. • Primordial(???) follicles: – Form before birth – Found in outer region of cortex – Each contains a SINGLE primary oocyte, surrounded by follicular cells (specialized epithelial cells) – No new primary follicles are formed during life. – Millions of oocytes at birth; 400,00 at puberty; 400-500 released during reproductive years Oogenesis: • The process of egg cell formation Follicular Maturation Ovulation • The process of releasing a secondary oocyte (18) and its associated polar body from the ovary Female Internal Accessory Organs 1. Uterine tubes 2. Uterus 3. Vagina 2. Uterine Tubes • Opens near the ovaries and travels medially into the uterus • Infundibulum (16): the funnelshaped end of the uterine tube at the ovary • Fimbriae (3): finger-like projections at the end of the infundibulum Uterine Tubes, continued….. • Oocytes are moved into and along the tubes by: – Ciliated epithelial cells – Peristaltic contractions • Fertilization occurs in the uterine tubes, and the oocyte becomes an egg (ovum) 4. Uterus • Hollow, muscular, pear-shaped organ • Located medially in the anterior portion of the pelvic cavity • Body of the uterus (22): upper 2/3 • Cervix (5): – lower 1/3 – Connects to vagina (6) • Cervical orifice (24): opening from uterus to vagina Uterine Wall 1. Endometrium(20)– mucosal layer 2. Myometrium(21) - _______ layer 3. Perimetrium(23) – serosal (thin, watery-filled) layer 6. Vagina • Fibromuscular tube that extends from the uterus to the outside of the body • Located posterior to urinary bladder (11) and urethra (12), and anterior to rectum (14) (see Fig. 19.7 diagram) • Functions: 1. Conveys uterine secretions 2. Receives penis during intercourse 3. Channel for birth Vaginal Wall 1. Inner mucosal layer • LACKS mucosal glands • Mucous comes from uterine glands and vestibular glands at mouth of vagina 2. Middle muscular layer • Mostly smooth muscle (involuntary) • Bulbospongiosus muscle (voluntary) closes off vaginal orifice (7) Vaginal Wall, continued….. 3. Outer fibrous layer – Dense connective tissue – Attaches vagina to surrounding organs • Urethra (13) • Rectum (14) Female External Accessory Organs 1. 2. 3. 4. Labia majora Labia minora Clitoris Vestibule 9. Labia Majora • Enclose and protect other external accessory organs • Correspond to male scrotum • Composed of 2 rounded folds of adipose tissue, smooth muscle, and skin that lie on either side of the other accessory organs • Anterior ends join to form the mons pubis 8. Labia Minora • 2 flattened folds that lie between the labia majora • Join with the labia majora posteriorly • Merge anteriorly to form a protective, hoodlike covering around the clitoris 10. Clitoris • Small projection at the anterior end of the vulva (the external accessory organs that surround the vaginal opening) • Corresponds to male penis: – 2 columns of erectile tissue (corpora cavernosa) – Glans, erectile tissue at anterior end, contains sensory nerve endings • So what would be its function? Vestibule • The space enclosed between the labia minora • Vestibular glands: – 2 at the opening of the vagina – Correspond to male bulbourethral glands (FUNCTION?) • Vestibular bulbs: – lie beneath the mucosa of the vestibule on either side – A mass of erectile tissue Erection , Lubrication, and Orgasm • Where is erectile tissue located? • Once these tissues are stimulated, parasympathetic nerve impulses release nitric oxide (a vasodilator). • What effect would a vasodilator have? • If stimulation is sufficient, vestibular glands secrete mucus into the vagina. (WHY??) Erection , Lubrication, and Orgasm, continued….. • The muscles of the perineum (area b/t the anus and external accessory organs) and walls of the uterus and uterine tubes contract rhythmically. • Why would all these areas need to contract? • Contractions help transport sperm to the upper ends of the uterine tubes. Hormonal Control of Female Reproduction Functions • Hormones are secreted by: – Hypothalamus – Anterior pituitary gland – Ovaries • Functions: – Control development and maintenance of female secondary sex characteristics – Maturation of female sex cells – Changes during monthly reproductive cycle Female Sex Hormones • About age 10, hypothalamus begins secreting GnRH, which stimulates _____________ to release _______ and _______. • Female sex hormones belong to 2 basic groups: – Estrogens (estradiol, estrone, and estriol) – Progesterone Estrogens • Produced primarily in the ovaries • Stimulate enlargement of ALL accessory organs • Develop secondary sex characteristics: – Development of breasts and ductile system of mammary glands – Increased deposits of adipose tissue subcutaneously and in breasts, thighs, and buttocks – Increased vascularization of the skin Progesterone • Also produced primarily in the ovaries • Promotes changes in the uterus during reproductive cycle • Affects mammary glands • Helps regulate secretion of gonadotropins from _________ gland Female Reproductive Cycle • AKA, menstrual cycle • Regular, recurring changes in the uterine lining • Ovarian cycle: changes in the ovaries (occurs along with menstrual cycle) • Menarche: female’s first menstrual cycle Female Reproductive Cycle, continued….. • Hypothalamus secretes ____________, which stimulates the _________ to secrete _______ and ______. • FSH stimulates maturation of an ovarian follicle. • LH stimulates ovarian cells to produce testosterone, which is used to produce estrogens. Female Reproductive Cycle, continued….. • Follicular cells produce estrogens: – Maintain secondary sex characteristics – Cause uterine lining to thicken • While follicle matures (1st 14 days of cycle), the estrogens secreted INHIBIT release of LH by the anterior pituitary gland. • Once follicle is mature, LH is released. Female Reproductive Cycle, continued….. • The released store of LH weakens and ruptures the bulging follicular wall, releasing the oocyte from the ovary. (What is this step called?) • The “empty follicle” fills with blood, clots, and forms a temporary glandular structure called the “corpus luteum”. • Corpus luteum secretes progesterone and estrogens. Female Reproductive Cycle, continued….. • Corpus luteum secretes progesterone and estrogens: – Progesterone causes the endometrium to become more vascular and glandular. – Estrogens and progesterones inhibit release of LH and FSH from _______, so no new follicles develop while corpus luteum is active. Female Reproductive Cycle, continued….. • If egg is unfertilized, corpus luteum begins to degenerate on about day 24 of cycle, becoming a “corpus albicans” • What would happen to estrogen and progesterone levels when the corpus luteum “dies”? • What do you think is the main source of estrogen and progesterone in a pregnant female? Female Reproductive Cycle, continued….. • In response to decreased levels of estrogen and progesterone, blood vessels in the endometrium constrict: – No more nutrients and oxygen to thickened uterine lining – Tissues die and slough off – Blood escapes from damaged capillaries Female Reproductive Cycle, continued….. • Because estrogen and progesterone levels are low, the hypothalamus and anterior pituitary glands are no longer inhibited, and cycle starts anew. Female Reproductive Cycle, continued….. • Figure 19.13, p.514 Menopause • The end of monthly cycles • Caused by aging of ovaries which, after about 35 years of cycling, contain too few primary follicles to have one mature each month. • Thus, no ovulation occurs, and blood levels of estrogen and progesterone plummet, causing changes in secondary sex characteristics. Mammary glands • Accessory organs specialized to secrete milk following pregnancy • Contained within the breasts • Mammary glands are composed of 1520 lobes, which contain alveolar glands that lead to an alveolar duct, which leads to a lactiferous duct, which leads to a nipple and opens to the outside. • Males have mammary glands which do not develop at puberty. (They lack ovarian hormones.) Critical Thinking 1. Why must the chromosome number be halved in sperm cells and oocytes? 2. Sometimes a sperm cell fertilizes a polar body rather than an oocyte. An embryo does not develop, and the fertilized polar body degenerates. Why is a polar body unable to support development of an embryo? Critical Thinking, continued….. 3. Some men are unable to become fathers because their spermatids do not mature into sperm. Injection of their spermatids into their partner’s secondary oocytes sometimes results in conception. A few men have fathered healthy babies this way. Why would this procedure work with spermatids, but not with primary spermatocytes? • What is the largest cell in the human body? • What is the smallest cell?